https://www.cbc.ca/news/canada/new-brunswick/cardy-fredericton-police-tweets-1.6323524
Cardy unleashes Twitter tirade against Fredericton police over planned protest
Cabinet minister asks police to call him to explain why 'illegal' protest is allowed under emergency order
In a series of posts on social media, Cardy called out the police force, asking why the "illegal" gathering is being allowed under the rules of New Brunswick's COVID-19 emergency order and suggesting their enforcement of the law is selective.
The posts began with a tweet on Thursday in response to a Fredericton police news release regarding the planned protest.
The release, posted on Twitter and on the force's Facebook page, noted that police are "aware of the planned rally" scheduled for Saturday afternoon at Fredericton City Hall.
"We have connected with the organizers of this event to discuss their intentions and make them aware of the possible consequences to gathering without following current public health measures," the release said, noting that officers will be recording the event via the force's drone and body-worn video cameras.
"We respect the right to peaceful demonstration, and our goal is to ensure public safety and security for all."
Cardy responded by asking police: "As a Fredericton MLA can you let me know how any sort of gathering is allowed under the Emergency Order, which specifically prohibits them?"
He later tweeted his phone number and said police should "feel free to call" him to clarify, "along with what other laws are optional in Fredericton if you decide you really don't like them."
On Friday afternoon, Cardy posted an announcement from the protesters' Facebook page, again calling out the Fredericton police.
"These folks think their rally tomorrow is okay, based on your message from yesterday," he said in a tweet.
"Please clarify that this gathering is illegal, and that there is no way to attend peacefully without risking a fine."
New Brunswick has been at the most restrictive level of its COVID management plan for a week, and it's to stay in lockdown at least until Jan. 30.
The police force has not publicly responded to Cardy's tweets or answered a CBC News request for comment, sent Friday afternoon.
Cardy did not respond to requests for an interview either.
 J.P.
Lewis, a political scientist at the University of New Brunswick in
Saint John, said that Cardy's latest tweets exemplify his unique and
'effective' social media strategy. (CBC)
J.P.
Lewis, a political scientist at the University of New Brunswick in
Saint John, said that Cardy's latest tweets exemplify his unique and
'effective' social media strategy. (CBC)
'Not unusual for Cardy,' political scientist says
But political science professor J.P. Lewis, who teaches at the University of New Brunswick in Saint John, said that a cabinet minister tangling with the police via social media isn't surprising — for Cardy.
"I think generally, we would describe it as unusual for a minister, but I wouldn't describe it as unusual for Dominic Cardy, just in terms of how he uses social media," Lewis said.
-
MLAs who voted 'No' on Cardy's vaccination bill ponder whether it's time to say 'Yes'
-
Education minister likens unvaccinated students to guns in schools
He noted that while cabinet ministers tend to use social media in very scripted and non-combative ways, Cardy has forged his own social-media style.
Cardy, whose pro-vaccination stance has been clearly and publicly established, was engaging in heated social media debates with anti-vaccination groups and individuals long before COVID-19 arrived, he said.
"We know that when the minister decides to turn up the volume politically … this is how he does it. And I think in the sense of bringing attention to it, it is effective," Lewis said.
Meeting protesters on their playing field
Taking his message to Twitter and directly targeting the group or the message he opposes "raises the stakes."
"By getting it out on social media, we know that brings a lot more attention compared to maybe traditional means of a minister releasing a press release saying 'I've contacted the local authorities and I'm concerned,' " Lewis said.
"If you tweet about it, it draws a lot more attention in this day and age."
There's also the advantage, whether deliberate or coincidental, that Cardy is meeting these groups "on their playing field," Lewis said.
Protesters rely on social media, particularly Facebook and Twitter, to spread their message, Lewis said.
"So he's engaging in that arena, basically."
Now that is truly too too funny
NDP gets help from democracy expert
CBC News · Posted: Jan 09, 2006 4:23 PM AT
An international expert on democracy has flown all the way from Egypt to help NDP candidate John Carty campaign in Fredericton.
Dominic Cardy is with a group called The National Democratic Institute. Its members include such people as former U.S. President Jimmy Carter. The group's mission is to teach democratic values and spread democracy around the world.
Cardy has taught about democracy in Algeria, Bangladesh, and Cambodia during the past few years. When he heard his friend John Carty was running for office back in his home town of Fredericton, he hopped on a plane.
"It was a strange experience," Cardy said. "One evening I was watching the sun go down over the pyramids, and the next evening watched it go down over Fredericton airport as I came into land."
Cardy is no relation to the NDP candidate. But he loves elections and loves getting people pumped up about democracy.
Carty the candidate is running against federal Indian Affairs Minister Andy Scott, Conservative Pat Lynch, Green candidate Philip Duchastel and independent David Amos. The riding has sent Scott to Ottawa for the last four elections, despite the best efforts of the other parties.
Cardy says he doesn't care how tough the race his – he just wants people to participate in the process. "People have forgotten how incredibly precious these gifts that our ancestors fought for are and were just giving them away. It makes me furious when I talk to people and people just say 'ah there's no point in voting.'"
After election day, Dominic Cardy is flying back home to his wife in Kathmandu, Nepal. He hopes to leave behind a new Member of Parliament for Fredericton, his friend John Carty for the NDP
I guess he supports people starving, losing their business, their home and their sanity. So why wouldn’t he support this.
Maybe you should take your own advice
No intelligent comments left?
I'm not a Higgs or Cardy fan but I do realize that they do have the power to enact laws that are enforceable no matter what you or I think. I'm on board to get rid of them as they've made a mess of things with this pandemic. They are however doing it legally. Luckily however we do have a way to get rid of them 1 vote per person.
At least you are knowledge about BS as you seem to use it often enough.
That should have been knowledgeable
should not have occured during such a serious moment
in covid transmission.......
legal but ethical?
A lot of unethical things going on with this Government but preventing these protesters in their "unethical" protests is in my best interest and I'm good with that. I will however be trying to get rid of them on election day.
That's yet to be seen. If your there today smile nicely you'll be on Police Camera's what do you suppose that's for?
Me thinks? Are you really D Amos?
That's up to law makers not union contracts between an employer and a union.
All Provincial and Federals laws supersede union contracts if they contain clauses are in fact against the law.
Making it up as you go.
https://www.cbc.ca/news/canada/new-brunswick/fredericton-council-tweets-social-media-1.6326340
Cardy's tweets about Fredericton police went too far, council says
Education minister's tweets about anti-lockdown protests 'inflamed' the situation
Fredericton city council says Education Minister Dominic Cardy's comments went too far last week, when he criticized the Fredericton Police Force for its response to a planned anti-lockdown protest.
Councillors voted Monday night to direct the mayor to send a letter to the province asking that "in the future, members of cabinet do not attempt to unduly impact policing decisions or inadvertently raise profile or risk levels for our citizens and police."
Mayor Kate Rogers said Cardy's comments had a negative impact.
"Anyone who followed the incident and social media around it and comments that were being made, I think it was very clear that it did further inflame the incident," Rogers said.
Rogers pointed out that another protest in Moncton didn't receive nearly as much attention.
"So one has to wonder," she said.
On Saturday, police said about 400 people rallied at city hall in downtown Fredericton to protest the New Brunswick government's COVID-19 lockdown measures.
Cardy's social media posts started on Thursday and continued on Friday, focusing on a force statement that the police respected the right to peaceful demonstration and were aware of the rally planned for Fredericton.
Cardy, who is MLA for Fredericton West-Hanwell, asked why police were allowing an "illegal" protest under the lockdown, which prohibits gatherings.
Fredericton Police Chief Roger Brown told council that Cardy spoke with the deputy police chief, Martin Gaudet, on Friday morning about the planned protest. Brown said Cardy wanted to "express his viewpoint" on what the police should do.
"And that's a very slippery slope," said Brown.
"We have the sole responsibility to answer the law, not to elected officials. And you know, that's something that is not helpful in any way, shape or form."
 A man was seen getting arrested by police during a protest
against COVID-19 restrictions in Fredericton on Saturday. (Aidan
Cox/CBC)
A man was seen getting arrested by police during a protest
against COVID-19 restrictions in Fredericton on Saturday. (Aidan
Cox/CBC)
"At the event itself — and we had lots of police officers on scene, as you saw — there were people there who clearly stated that they were there at the request of Minister Cardy to protest the protesters."
Two people were arrested at the protest on Saturday and several tickets were issued to organizers and participants at the rally for violating the Emergency Measures Act, according to police.
"It is a big task to contain a protest during a pandemic and that work alone is enough and it doesn't need to be fuelled and inflamed by anyone," said Rogers. "And we would particularly ask our partners at the province to respect that."
Brown said he was disappointed in Cardy's comments.
"In my policing career I've often been held to account for whether it be the actions of the entire police force or myself. And in this particular case, I think elected officials also need to be held to account for their roles."
https://www.cbc.ca/news/canada/new-brunswick/fredericton-protest-covid-19-restrictions-1.6324377
Protesters, police clash during Fredericton rally against COVID-19 restrictions
2 protesters arrested, others attempted blocking police cruiser
Police and protesters clashed outside Fredericton city hall during a protest against COVID-19 restrictions Saturday afternoon.
Police say there were two arrests.
The downtown rally began at about 1 p.m. Hundreds of people assembled at the corner of Queen and York streets, many unmasked, with some carrying signs indicating opposition to government-imposed restrictions and vaccination mandates.
Police say about 400 people attended the rally, with uniformed officers from the Fredericton Police Force and the Department of Justice and Public Safety in attendance.
At about 2 p.m., an argument broke out between a small group of protesters and officers. A man could later be seen being escorted away in handcuffs.
 Two men were arrested during a protest against COVID-19 restrictions in Fredericton on Saturday. (Aidan Cox/CBC)
Two men were arrested during a protest against COVID-19 restrictions in Fredericton on Saturday. (Aidan Cox/CBC)
Other protesters followed as the man was led into a police vehicle parked on Queen Street.
Moments later, another man was seen in a scuffle with officers near the vehicle before being taken to the ground and held down by several police officers.
As police prepared to drive away with the first man who was arrested, protesters swarmed the vehicle, prompting other officers to move in and push them away.
Police were later seen picking up the other arrested man off the ground and walking him to the police station further down the street.
In an email Saturday evening, Fredericton Police Force spokesperson Alycia Bartlett confirmed two men were arrested during the protest.
Bartlett said the men are facing a number of criminal charges in addition to fines for failing to follow the province's Emergency Measures Act.
 A
man attempted to prevent another protester from being arrested at
Saturday's protest against COVID-19 restrictions. He was subsequently
tackled, handcuffed by officers and walked to the police station just
down the street. (Shane Fowler/CBC)
A
man attempted to prevent another protester from being arrested at
Saturday's protest against COVID-19 restrictions. He was subsequently
tackled, handcuffed by officers and walked to the police station just
down the street. (Shane Fowler/CBC)
Bartlett said several other tickets were issued to organizers and participants at the rally for violating the Emergency Measures Act. Other individuals have been identified and will be issued tickets "promptly," she said.
She shared a brief written statement from Fredericton Police Chief Roger Brown, who said it was unfortunate that organizers continued to promote the event despite the pandemic affecting so many in the community.
"The tickets issued for those involved demonstrates the importance of holding to account those who continue to ignore the rules, putting public health and safety at risk," Brown stated.
Bartlett said the force had encouraged organizers against gathering ahead of the protest.
She said the protest was mostly peaceful, but added there was "a small group of citizens who acted to incite dissension, creating a dangerous and potentially violent situation."
 Police say about 400 people gathered outside of Fredericton
city hall for a protest against COVID-19 restrictions on Saturday.
(Shane Fowler/CBC)
Police say about 400 people gathered outside of Fredericton
city hall for a protest against COVID-19 restrictions on Saturday.
(Shane Fowler/CBC)
The protest was held despite New Brunswick being in Level 3 of its COVID-19 Winter Plan, which prohibits public gatherings.
It also went ahead following criticism from a New Brunswick cabinet minister toward the Fredericton Police Force over messaging around how the protest would be handled.
In a series of tweets beginning on Thursday, Education and Early Childhood Minister Dominic Cardy called out the police force, asking why the "illegal" gathering was being allowed under the rules of New Brunswick's COVID-19 emergency order, and suggesting their enforcement of the law is selective.
It was in response to a statement the force issued on its social media channels on Thursday saying it was aware of the planned protest, and that the force had contacted the organizers to discuss their intentions and inform them of possible consequences of gathering without following public health measures.
"We continue to take a measured approach to encourage and promote compliance with COVID-19 guidelines to reduce the spread of the virus," the force's statement said.
"Tickets or other enforcement action is possible if organizers or participants are not following public health directives."
Protesters on Saturday said another protest was planned for Moncton on Sunday.
Heroes of the pandemic: New Brunswick politician who crushed the COVID-19 curve is a virus whisperer
Dominic Cardy saw the virus coming back in late December and put together an action plan for the province by February
 The coronavirus, which he first heard about while on vacation in Costa Rica, instantly grabbed Dominic Cardy’s attention. Photo by THE CANADIAN PRESS/Marc Grandmaison
The coronavirus, which he first heard about while on vacation in Costa Rica, instantly grabbed Dominic Cardy’s attention. Photo by THE CANADIAN PRESS/Marc Grandmaison Dominic Cardy did something he almost never does last Christmas and went to Costa Rica for a holiday, his first vacation, of any kind, in years. Costa Rica had sun, beaches, tropical fruit drinks and, as it turns out, the BBC World News channel reporting on an unidentified pneumonia in China.
The story instantly grabbed Cardy’s attention. The 49-year-old Minister of Education for New Brunswick was, in his words, a “weird kid,” with some weird interests, including plagues. Cardy remembers visiting his grandmother in England and going to a church cemetery to check out the “plague pits,” mass graves used to bury victims of the Great Plague that swept over England in 1665-66.
“My grandmother had a copy of Journal of a Plague Year by Daniel Defoe,” Cardy says. Naturally, he read the book, and others, and when the BBC story about a mysterious illness interrupted his holiday bliss, he started digging for more information, calling his contacts, some in public health, that he met while working in Southeast Asia for a not-for-profit promoting democracy.
Cardy’s friends overseas were worried, which made him even more worried, and doubly so since the stories of the strange new illness were emerging from China, a country with a government that isn’t famous for its transparency.
“History is filled with people who spend their time just before a crisis hits saying, ‘It is overblown, what could possibly go wrong?’ ” Cardy says.
In New Brunswick — with 120 confirmed COVID-19 cases,
118 recoveries, no deaths and no active cases currently in hospital —
it has been a story of what could possibly go right, and Cardy deserves a
good deal of credit for it. The province was the first to lockdown, and
has been one of the first to open up again. Its nursing homes didn’t
become COVID-horror shows. Its government hit it out of the park.
When Canada’s chief public health official, Dr. Theresa Tam, was talking about there being no need to “panic,” and raising alarms instead about the internet-wacko fringe targeting Canadians of Chinese descent with racist comments on social media in late January, a little known Progressive Conservative education minister in a small Maritime province was fully panicking. Cardy was preparing to pitch his premier’s top aide on the need to take drastic action to stop a killer virus.
Cardy, indeed, kept watch on the news out of Asia upon his return from Costa Rica. When he was invited to two Super Bowl parties in early February, he went to the one hosted by Louis Leger, chief of staff for his boss, Premier Blaine Higgs. Cardy doesn’t know anything football. But he knew enough to grab some couch-time next to Leger.
 New Brunswick Progressive Conservative MLA Dominic
Cardy, left and New Brunswick Progressive Conservative MLA Jake
Stewart, talk prior to the Throne Speech at the New Brunswick
Legislature in Fredericton, N.B., on November 20, 2018. Photo by THE CANADIAN PRESS/James West
New Brunswick Progressive Conservative MLA Dominic
Cardy, left and New Brunswick Progressive Conservative MLA Jake
Stewart, talk prior to the Throne Speech at the New Brunswick
Legislature in Fredericton, N.B., on November 20, 2018. Photo by THE CANADIAN PRESS/James West
Leger asked, what worried him most?
“We are in a minority government with all sorts of political challenges and I think that was what Louis was expecting me to answer, but I said, I am worried about this new virus. And he said, ‘Really?’ ”
Cardy kept on talking, and over the next few weeks, he and Leger would talk some more, until the premier’s staffer asked him to put together a report on the virus and be prepared to present it at a caucus retreat on Feb. 24.
The resulting white paper is a 19-page, 4,412-word, action-oriented masterwork. Cardy wrote it in the living room of his apartment over a seven-hour burst on a Sunday with the help of his girlfriend, Julia Smith, and two fact-checkers, one of whom was Cardy’s younger sister, Vanessa, a doctor.
“The COVID-19 virus will arrive in New Brunswick and may be already present given the unreliability of tests, the weakness of Canada’s public health response to date and the nature of our open society,” Cardy wrote. “This is not a question of if, but when.”
This is not a question of if, but when
The paper touches on super spreaders, transmission rates and asymptomatic carriers. It recommends adopting an “executive cabinet,” to include the leaders of the opposition parties, delaying municipal elections, encouraging private sector workers to work from home, converting school gymnasiums into infection-detection centres and possibly quarantining nursing homes.
Pre-virus budget projections were to be discounted, while the government, above all, was to be transparent and consistent in its messaging to get public buy-in on the restrictive measures to come, and to counteract the noise and virus-related misinformation swirling about on social media.
As an added narrative twist, Cardy, the guy sounding the alarm, was a turncoat of sorts, a former leader of the New Brunswick NDP (true story!) who switched teams and got elected as a Conservative. Now, here he was, hollering from the political mountaintop, albeit behind closed doors, that if the Higgs’ government didn’t take the virus seriously the fallout would be catastrophic.
After his presentation the premier asked Cardy what he would do. “Shut everything down,” was his reply.
“This was late February, and if we had done that, people would have thought we were crazy,” Cardy says.
 New Brunswick Premier Blaine Higgs speaks with the media in Fredericton on Feb. 17. Photo by Stephen MacGillivray/The Canadian Press
New Brunswick Premier Blaine Higgs speaks with the media in Fredericton on Feb. 17. Photo by Stephen MacGillivray/The Canadian Press
On March 1, premier Higgs issued a statement addressing the virus,
urging all travellers returning to New Brunswick to monitor themselves
for symptoms. Schools closed soon after, businesses and international
borders followed, while checkpoints were adopted at provincial borders.
All non-residents and non-essential workers could be turned away.
Cardy, the canary in a COVID coal mine, initially came under fire from the New Brunswick Medical Society, for pushing measures some physicians perceived as overly drastic steps.
In hindsight, he wishes the steps had been taken weeks earlier. “There is a sadness that people like me weren’t able to be louder earlier to hold off on some of the deaths and limit the damage to peoples’ lives and the economy we are seeing,” he says.
In late April, just as Toronto was closing one of its largest city parks, New Brunswick was creaking to life again. Premier Higgs triggered phase one of a four-phase recovery plan on April 24, allowing access to golf courses and permitting families to join forces with a second family, creating so-called two-family bubbles.
"We have managed to push the virus back out of the city walls, but it is still there, outside the city walls, trying to get in"
Phase two kicked in May 8. Elective surgeries are to resume, and outdoor gatherings of up to 10 people are allowed — with social distancing. Museums and businesses are opening, beaches and ATV trails, too. Schools will remain closed until September, however, and the education minister fully expects a mix-bagged of a fall to come, blending open classrooms — with online learning at home — depending on where things stand in the fight against a virus that he started.
“It is like a medieval siege,” Cardy says, reaching for a metaphor from an earlier age of plagues and books by Defoe. “We have managed to push the virus back out of the city walls, but it is still there, outside the city walls, trying to get in.
“We are not going to be able to hold it off at all points at all times, so that’s why we have to make sure we are as careful as we can be.”
• Email: joconnor@postmedia.com | Twitter: oconnorwrites
https://www.macleans.ca/longforms/covid-19-pandemic-canada-year-one/

A message board over a highway in Halifax on Tuesday, April 21, 2020. (Darren Calabrese)
Year One: The untold story of the pandemic in Canada
A comprehensive report on the country's mishandling of the crisis of the century
We gave our entire April 2021 issue over to a single piece, written by Stephen Maher and edited by Sarmishta Subramanian. The 22,000-word story is the most comprehensive accounting yet of what went wrong, and right, in our nation’s handling of the pandemic. Learn more about why we did it. After a limited release to newsletter subscribers, we are making it available in full for free here.
Chapter One: A danger dawns
‘Everybody knows that pestilences have a way of recurring in the world; yet somehow we find it hard to believe in ones that crash down on our heads from a blue sky. There have been as many plagues as wars in history; yet always plagues and wars take people equally by surprise.’
—Albert Camus, The Plague
In the last hours of 2019, Dominic Cardy and Julie Smith checked into the Arenal Observatory Lodge & Spa, a hot spring resort in La Fortuna de San Carlos, Costa Rica, with a view of the spectacular Arenal volcano, which rises out of a rainforest full of waterfalls, howler monkeys and exotic birds. Their room wasn’t ready when they arrived, so they took the hotel clerk’s suggestion and had a drink in the bar. “And it flashed up on the screen that there had been the first suspected transmission,” Smith recalled later.
Smith heads a literacy organization in New Brunswick, but for 10 years she worked for the federal government, mostly in Ontario, doing policy work in areas including counterterrorism. Her boyfriend, Cardy, has been the New Brunswick education minister in the Progressive Conservative government of Blaine Higgs since 2018, but for many years he worked in the developing world for the National Democratic Institute. Self-described policy wonks, they like to unwind by talking about news and ideas, even when they are drinking tropical cocktails in a Costa Rican forest. “So we spent the night in hot tubs, and as normal humans do, spent our New Year’s Eve talking about COVID,” Smith said.
The disease was not then known as COVID-19. (The World Health Organization gave it that name in February.) Few people were thinking about it outside of China. The TV report that Smith and Cardy saw that day in Costa Rica would have been among the first international media reports on the virus, the result of a bulletin issued the day before by ProMED, a volunteer-run information service alerting scientists and doctors of infectious disease outbreaks.
The message, titled “UNDIAGNOSED PNEUMONIA – CHINA (HUBEI): REQUEST FOR INFORMATION,” laid out the earliest news out of Wuhan for ProMED’s 80,000 subscribers:
On the evening of [30 Dec., 2019], an “urgent notice on the treatment of pneumonia of unknown cause” was issued, which was widely distributed on the Internet by the red-headed document of the Medical Administration and Medical Administration of Wuhan Municipal Health Committee.
On the morning of [31 Dec., 2019], China Business News reporter called the official hotline of Wuhan Municipal Health and Health Committee 12320 and learned that the content of the document is true.
The report was based on a Google translation, which explains why a red notice was called a “red-headed document.” It described four patients with fever, in acute respiratory distress that failed to respond to antibiotic treatment. Dr. Li Wenliang, a 33-year-old ophthalmologist at Wuhan Central Hospital, had sent messages to a private WeChat group warning medical school classmates: “There are seven confirmed cases of SARS at Huanan Seafood Market. The latest news is, it has been confirmed that they are coronavirus infections, but the exact virus strain is being subtyped. Protect yourselves from infection and inform your family members to be on the alert.”

Coronavirus patients wait to be transferred to a newly built hospital in Wuhan, China, in early March 2020 (STR/AFP/Getty Images)
When someone posted Li’s message on a bulletin board, Western virus watchers were alerted, and so were Chinese police. They detained Li and seven other medical staff for violating a Chinese law against spreading rumours. They forced Li to issue a statement retracting his warning. He was allowed to return to his hospital, where he contracted the disease, which killed him on Feb. 7. He is now celebrated as a hero in China and around the world.
Early on Dec. 31, the Reuters news agency in Beijing reported that the Wuhan Municipal Health Commission was investigating 27 cases of viral pneumonia. Chinese officials reported the outbreak to the World Health Organization (WHO), and global media organizations started to take notice. The same day, authorities closed the market in the heart of Wuhan (population 11 million) that had been identified as the locus of the outbreak.
On the other side of the world in Costa Rica, Cardy and Smith read everything they could find about the mysterious virus. “I remember raising it with her, [saying] ‘This doesn’t look good,’ ” said Cardy. “All those things you look for that usually make the initial scare around a disease somewhat less scary once there’s more science and data—in this case, every single day, every single new piece of information made COVID seem like it was going to be much more viral.”
Smith was living in Ghana when Ebola broke out in neighbouring countries, when Ghanaians were petrified it was going to spread to their country. She and Cardy were both aware that security experts believed the world was at risk from a new global pandemic—something they had learned at conferences and in their readings—so as they continued their Costa Rica vacation, they talked about the policy implications.
“I think we were unpacking that expectation that we were going to have the 100-year sort of thing, that we were due for a big pandemic,” said Smith. “Were we ready? This could be really bad. It could be the one.”
***
If it was going to be the “one,” the world-shaking pandemic that experts had warned was coming, Canada seemed well-positioned to handle it. After being tested by the SARS outbreak in 2003, Canada had put some effort into building up its public health capacity. And the country was governed by Justin Trudeau’s Liberals, who had campaigned on ending the Conservative “war on science.” The virus didn’t have an ally in this country the way it did in the United States, with a commander-in-chief and state-level politicians who questioned the science and resisted mitigation measures even when tens of thousands were dying.
Canadians could also be reassured by the presence of Dr. Theresa Tam, at the Public Health Agency of Canada (PHAC). Tam, the chief public health officer of Canada, seemed the perfect leader for the challenge. Born in Hong Kong and raised in the United Kingdom, she has deep experience with Asia and respiratory diseases. She was chief of respiratory disease at PHAC’s Centre for Infectious Disease Control and Prevention, and working for the agency in 2003, when a Toronto woman contracted SARS on a trip to Hong Kong and brought it back to Canada. It quickly spread through an ill-equipped Ontario health system.
Tam also literally wrote the book on how Canada should manage a pandemic. In 2006, she co-authored “The Canadian Pandemic Influenza Plan for the Health Sector,” a complex, detailed 550-page road map for Canada facing a viral invasion. Tam consulted dozens of doctors, academics, public health officials and other stakeholders, and warned of the risk Canada faced.
With that experience, her 55 peer-reviewed papers and years of high-level experience as an expert with the WHO, Tam would have been among the people in the world best-placed to understand the threat from the mysterious viral pneumonia spreading in Wuhan.
In early 2020, Tam did not yet see evidence that the new coronavirus that was panicking officials in China was going to reach Canada. On Jan. 7, PHAC issued a mild travel warning, merely asking Canadians visiting Wuhan to “avoid high-risk areas such as farms, live animal markets, and areas where animals may be slaughtered.” It’s not that Canada wasn’t paying attention. “Right now we are monitoring the situation very carefully,” said Tam. “There has been no evidence to date that this illness, whatever it’s caused by, is spread easily from person to person; no health-care workers caring for the patients have become ill, a positive sign.”
On Jan. 21, while Trudeau was in Winnipeg for a caucus meeting, he made headlines, not over the coronavirus, but for buying boxes of fancy doughnuts at a local shop rather than at a chain. Tam had reassured Canadians the previous day: “It is important to take this seriously and be vigilant and be prepared, but I don’t think there’s any reason for us to panic or be overly concerned.” The country was much better prepared since SARS, she suggested. “From my perspective a lot has changed from 2003, and we are in a better position to respond to a variety of emerging infections.”
In China, the virus was spreading. By then, there were 278 cases of mysterious pneumonia, the vast majority in Wuhan. There were four cases outside China, in Thailand, Japan and South Korea. The day before, senior Chinese leaders, alarmed by the spread of the illness, had ordered Wuhan locked down. Worryingly, the Wuhan Municipal Health Commission had reported that 15 health-care workers in the city had been diagnosed with the illness, a clear sign it was spreading between people. In nearby Taiwan, officials intensified the airport screening they had already implemented weeks earlier.
But in Canada and elsewhere, the virus continued to be a remote concern. On Jan. 23, Tam was among the dozen expert advisers who helped WHO director general Dr. Tedros Adhanom Ghebreyesus decide it was not yet time to declare the coronavirus “a global health emergency.”

An X-ray that showed diffuse opacities throughout a patient’s lungs led doctors to identify the first known case of COVID-19 in Canada (The Lancet/Elsevier)
That evening, the novel coronavirus made its debut in Canada. A 56-year-old man who had recently travelled to Wuhan was admitted to Sunnybrook Health Sciences Centre in Toronto. He had a temperature of 38.6° C, a low-grade fever, and was congested. Dr. Jerome Leis, medical director of infection prevention and control, was watching for patients who fit the risk profile. He had an X-ray of the patient’s lungs sent to his home. One look told him what he was dealing with.
“There were diffuse opacities throughout both lungs in different regions of a patient who really only had a few days of symptoms,” he said. “So I thought that was quite striking. Usually, if you hear about someone who’s got a bit of a cold, we don’t expect to see those types of lower lung abnormalities so quickly.”
The hospital sent a blood sample in a taxi to Public Health Ontario’s laboratory, where technicians had been frantically working with information from China to develop a test for the virus. Once Sunnybrook got the result, Dr. Lynfa Stroud, division head of general internal medicine at Sunnybrook, and Leis went to the ward to let staff know they were looking after Canada’s first novel coronavirus patient.
It was a dramatic moment for nurse Kathryn Rego. “They came up to the nursing station and we went into this tiny little room and squished all of ourselves in, and that’s also not a common thing, that every single person on a unit stops,” she said. “The cleaners, our support staff, everyone stopped what they were doing, just squished into this room to hear that this guy was positive.”
The news that they were caring for a coronavirus patient was startling, but not unexpected. Sunnybrook had prepared for the possibility. When Clarice Shen, a nurse in her third month on the job, showed up at work that day she discovered she had been assigned to a “closed” room in the general internal medicine ward, with no patient. Confused, she asked a supervisor about it, and was told the room was reserved in case a patient came in with the novel coronavirus. It was a negative pressure room, one of eight the hospital had set up after SARS, where a patient could be kept in isolation, following protocols for any novel pathogen. A few hours later, she had a patient: the man who had travelled to Wuhan. Shen volunteered to work more shifts so she could care for him, because they could both speak Mandarin. The man had a mild case. He spent a week in hospital, and was discharged.
For Canada, the story was just beginning. There were four confirmed cases by the end of that month; 20 by the end of February; and 8,589 by the end of March. A year after that first patient checked into Sunnybrook, there would be 747,110 confirmed cases in Canada and 19,009 deaths. But already, by that January evening, the microbe known as SARS-CoV-2 had begun its remorseless spread, following its viral logic. Viruses want only to replicate, to find new hosts and fresh lung tissue to infect. To stop them, to curb transmission, societies must follow a narrow path. A few countries succeeded in doing this in that vital first month. Canada did not. It was the first failure of many, setting the country up for a year of challenges we would struggle to meet.
***
In New Brunswick, Dominic Cardy and Julie Smith were worried. Since returning from Costa Rica, they had been tracking news about the coronavirus, texting each other links to stories. On Jan. 23, the same day the patient arrived at Sunnybrook, Smith travelled to Ottawa. Cardy texted her reminders to avoid touching her face. He sent a link to a cellphone video taken in a Wuhan hospital showing patients suffering on gurneys in hallways. “The stuff coming out of China is worrying,” he wrote. “Have you seen the videos? People collapsed in the streets etc.”
“I basically tried not to touch anything at the airport and have used Purell three times this morning already,” Smith replied.

Cardy (left) and Smith sounded the alarm early about the threat that the coronavirus posed to New Brunswick (Photograph by Jordan MacDonald)
By then, 655 cases had been confirmed around the world, and 95 people were severely ill. There were now cases in Hong Kong, Macau, Taiwan and the United States. The virus was spreading in Guangdong province among people who had not travelled to Wuhan. A WHO situation report on Jan. 23 contained a sense of growing urgency. “WHO assesses the risk of this event to be very high in China, high at the regional level and moderate at the global level,” it said; the global risk level was corrected afterward to high.
In the U.S., President Donald Trump was briefed, and on Jan. 24, Congress had its first coronavirus meeting. U.S. classified intelligence briefings, which would presumably have been shared with Canada’s leaders, were warning of a possible global pandemic. The medical community, too, was publicly sharing dire warnings. On Jan. 27, Dr. Gabriel Leung, dean of the University of Hong Kong medical school and a graduate of the University of Western Ontario, made headlines around the world when he revealed modelling showing the virus was much more widespread than China had acknowledged. He followed it up with a Lancet article a few days later telling the world to get ready for COVID-19: “Independent self-sustaining outbreaks in major cities globally could become inevitable because of substantial exportation of presymptomatic cases and in the absence of large-scale public health interventions. Preparedness plans and mitigation interventions should be readied for quick deployment globally.”
On Jan. 30, the WHO finally declared “a public health emergency of international concern,” which didn’t stop China from pressuring other countries to keep their borders open.
Cardy and Smith followed these developments with concern. On Feb. 2, Cardy got the opportunity to do something about it. Louis Léger, the chief of staff to Premier Blaine Higgs, had invited Cardy to his place in Fredericton to watch the San Francisco 49ers and the Kansas City Chiefs in the Super Bowl. Cardy, who doesn’t care for football, jumped at the chance, because he wanted to use it to convince Léger that New Brunswick had to start getting ready for the virus.
Cardy went to Léger’s home, where they watched the game with Léger’s daughter. Eventually, talk turned to politics. “He started off by asking, ‘What’s worrying you?’ ” said Cardy. Léger admits he was expecting a normal discussion about politics. “At that time we were in a minority situation, with all the complication of a minority, the house coming back with a budget,” Léger recalls. Instead, Cardy launched into a discussion of COVID-19. “He was genuinely very preoccupied by it,” Léger recalls. “He was reading, reading, reading, and I think he saw it coming.”
Persuaded by the urgency of Cardy’s observations, Léger asked him to write a report for the premier. Cardy and Smith set to work on it together, in their Fredericton condo. They enlisted the help of Cardy’s sister, Vanessa Cardy, a family doctor who practises in Wakefield, Que., near Ottawa, and in the Cree community of Chisasibi, on James Bay.
Smith was sure the federal government was failing to act quickly enough, imposing travel guidelines after the virus had already moved and constantly struggling to catch up. It was a pattern that would continue. “If you actually read the news, Italy has collapsed because of this. But people can still come from Italy,” she said. “And then we finally deal with Italy, but it’s in the States. It always felt like the response was behind.”
Cardy wanted to make sure that New Brunswick didn’t end up like many other places in the world, where officials learned with horror that their hospital ICUs were suddenly full.
The virus had spread to 32 countries and there were soon worrying indications that officials in Iran and China were hiding the extent of transmission. At a caucus meeting on Feb. 24, Cardy delivered a grim 4,000-word report explaining the risk he saw. He described the impact of “superspreaders,” like the South Korean woman who had infected dozens by attending a church service while symptomatic—a phenomenon that would, months later, become the focus of intense study. He outlined the threat and laid out steps New Brunswick could take using emergency legislation to contain the virus.
“The COVID-19 virus will arrive in New Brunswick,” his paper argued, “and may be already present, given the unreliability of tests, the weakness of Canada’s public health response to date and the nature of our open society. This is not a question of if, but when. COVID-19 will kill some New Brunswickers, infect many others and disrupt the operation of government, the economy and the lives of all citizens. The extent of the damage and disruption cannot yet be predicted, but it will occur. Government will be judged on their handling of this crisis.”
Cardy had convinced the premier. But some public health people were reluctant, he said. “I still remember one of them saying . . . one of the sections in my paper was how to manage a pandemic. And he’s like, well, the first thing politicians need to know is that they shouldn’t manage pandemics. That’s our job.”
Cardy, who was right when a lot of other people were wrong, thinks it was difficult for politicians and health officials—in Fredericton, Ottawa and across the country—to accept the urgency of the situation. “There was a tendency from elements of the bureaucracy that have high levels of trust but had very little experience dealing with anything similar in recent decades, coupled with a political class that’s feeling pretty beleaguered and disconnected and being knocked back and forth by populist movements from left and right. When you combine all those things, it led to a pretty slow and piecemeal and not very well-targeted response, because in Canada, we were weeks and weeks after everyone else was talking about asymptomatic spread.”
Cardy was determined to keep the virus out of New Brunswick. He and Smith connected with Roxann Guerrette, a 30-year-old scientist who was working on her Ph.D. at the Université de Moncton, who was also worried, and they started exchanging ideas about how they could goad a reluctant bureaucracy and an unaware public into action. They had a fight ahead of them, and they still carry the scars, but as of February 2021, New Brunswick has lost only 27 people to COVID. Neighbouring Maine lost 703 and Quebec a horrifying 10,393.
***
In her 550-page pandemic plan, Tam had predicted what was about to happen. “The next pandemic virus will be present in Canada within three months after it emerges in another part of the world, but it could be much sooner because of the volume and speed of global air travel,” she wrote. “A pandemic wave will sweep across Canada in 1-2 months affecting multiple locations simultaneously. This is based on analysis of the spread of past pandemics including the 1918 pandemic.”
Tam knew what to look for, but in January 2020, she was either not seeing it coming, or not making her fears public. She had had experience dealing with SARS, which killed 44 Canadians before it was wrestled under control. In 2005, Tam and five colleagues published a research paper on screening measures—questionnaires and thermal scans—used in Canadian airports during that outbreak with a goal of preventing passengers with SARS from introducing it to Canada. Tam and her colleagues found that although the Canadian government spent $7.6 million on the effort, it did not detect a single case.

Chief Public Health Officer Dr. Theresa Tam in Ottawa on March 23, 2020; early messaging prioritized hand sanitizing, not masks (Blair Gable/Reuters)
Tam knew what worked and what didn’t, knew what resources Canada had, knew the players here and around the world, and knew how a pandemic would behave. She has been a reassuring TV presence throughout the pandemic, delivering succinct public health messages in her mid-Pacific accent, which sounds as if it was picked up at health conferences. She’s not a dynamic speaker, but she is approachable. She told children in a CBC Kids interview that her song of choice for handwashing is “We will, we will, wash you,” to the tune of the Queen classic.
Tam comes across as calm and determined, unflappable, trustworthy, the right person for the job. But she seems to have been wrong about a number of things when it would have been good to be right. In early 2020, her agency repeatedly said the risk of an outbreak in Canada was low. On Jan. 6, a spokesman for PHAC told the Ottawa Citizen that Tam was monitoring the issue, but Canada was well-prepared, in part because of public health systems that would “identify, prevent and control the spread of serious infectious diseases into and within Canada.” Health Minister Patty Hajdu, too, made similar reassuring statements.
Early interventions were modest. On Jan. 22, the government moved to screen passengers from Wuhan at three Canadian airports. When Liberal MP Marcus Powlowski, a Thunder Bay ER doctor, asked Tam in a health committee meeting if it might make sense to ask travellers returning from China to isolate for two weeks, given the virus had moved beyond Wuhan and there were newspaper reports of asymptomatic transmission, Tam said no, bolstering her initial statement that, “for other completely asymptomatic people, currently there’s no evidence that we should be quarantining them.” Hajdu told a teleconference with provincial counterparts that “the risk to Canadians remains low.”
Even after the WHO declared COVID an emergency on Jan. 23, 2020, Tam was warning Canadian leaders against quarantines or travel restrictions, in keeping with WHO guidelines. Tedros had warned countries not to restrict travel more than was necessary: “We call on all countries to implement decisions that are evidence-based.”
Looking back with the benefit of hindsight, it is striking that many public health experts believed COVID-19 could be managed like previous threats—SARS, MERS, swine flu—that flared up, capturing headlines and provoking anxiety before being suppressed. COVID-19, with its easy person-to-person transmission and its long period of asymptomatic spread, would not be stopped as easily.
The same day Hajdu spoke to provincial ministers, Tam warned healthy Canadians against wearing masks. “Sometimes it can actually present risks as you are putting your fingers up and down your face when removing your mask and putting them near your eyes,” she said. She was not alone in this; at that time, neither the WHO nor the U.S. Centers for Disease Control and Prevention (CDC) were recommending that the public wear masks, either because the research was unclear on whether it was protective, or because officials feared that hoarding would disrupt the supplies needed in hospitals. In any case, masks would, of course, become a vital piece in slowing transmission.
Meanwhile, the virus moved around the world. University epidemiologists were sounding alarms. And there were countries, particularly in Asia, that were taking the threat seriously, and using the mask policies and border controls that the WHO and Canada were still not recommending. In early January, before there was a single domestic case, Vietnam’s government began monitoring the outbreak’s progress within China and, before long, introduced quarantines at airports, seaports and land borders. On Feb. 3, Japan ordered the cruise ship Diamond Princess quarantined in Yokohama after COVID was confirmed in a passenger who had disembarked in Hong Kong; soon there would be hundreds of infected passengers aboard. Researchers eventually revealed that asymptomatic passengers were carrying the disease, providing an illustration to media consumers around the world of the pernicious nature of the virus. On Feb. 5, Taiwan announced that Chinese nationals were banned from entering the nation; all other travellers had to quarantine for 14 days. By the end of the month, many schools in Japan had closed. After an outbreak in South Korea, the government there declared a red alert on Feb. 23, and other countries started imposing restrictions on Korean travellers.
By late February, the crisis had moved beyond Asia. Outbreaks were appearing in small Italian towns. Venice brought its carnival to an early close and the Italian government suspended sporting events.
All along, in Canada, the government was emphasizing the need for social harmony. There is a long, grim history of ethnic groups being scapegoated during disease outbreaks, and Trump’s anti-China messaging targeted Asians. Incidents of hate surged in the United States in 2020, and the Vancouver Police Department reported a spike in anti-Asian hate crimes in that city.
That well-grounded fear, rather than the threat of a virus that would ultimately take a terrible toll on racialized Canadians, seems to have been top of mind for Canadian leaders early in 2020. At a health committee meeting in Ottawa on Jan. 29, Tina Namiesniowski, then the president of the Public Health Agency of Canada, told MPs the government needed to take care to avoid targeting communities. “This is a vital lesson we learned from our experience with SARS, when a situation arose in which some Chinese communities and individuals were the victims of racism and racial profiling. We must confront that problem,” she said. Tam, in answering MP Powlowski’s question about travellers from China, echoed that message. “The global effort to contain the virus requires the absolute commitment and engagement of the communities that are affected. Otherwise, they’ll be stigmatized,” she said.

Some critics have wondered whether Tam and PHAC had enough independence from government (Adrian Wyld/CP)
Likewise, Trudeau’s first substantial comments about the virus came at a Chinese New Year dinner at a banquet hall in the Scarborough neighbourhood of Toronto on Feb. 1. “There is no place in our country for discrimination driven by fear or misinformation,” he said to applause.
There are indications that behind the scenes the federal government was starting to see the danger. On Feb. 3, as part of preparations for an emergency flight to airlift Canadians out of Wuhan, the Trudeau government made an order-in-council declaring that COVID-19 posed “an imminent and severe risk to public health in Canada.” But although the government had reached that conclusion, it was not behaving as if it was worried. During a teleconference with provincial health ministers and officials—leaders who would before long be struggling with the most serious pandemic to hit Canada in a century—Tam appears to have been focused on keeping everyone calm. “Having been part of the WHO Emergency Committee’s deliberations,” she said, “I can say that the decision to declare a Public Health Emergency of International Concern was based on the need to enhance preparedness and response in vulnerable countries in particular, given the potential for the outbreak to overwhelm their health systems.”
In February, Canada shipped 16 tonnes of masks, goggles, face shields and other personal protective equipment (PPE) to China to help it contain the virus. China, which as the year went on was less and less helpful to Canada, thanked us for the equipment, but before long, people in Canadian long-term care homes were dying in part because staff didn’t have masks. We later learned the federal and Ontario governments had also let PPE emergency stockpiles dwindle, discarding them when they expired rather than replacing them. A CBC investigation discovered that two million N95 masks and 440,000 medical gloves were landfilled in 2019.
As February drew to a close, it was becoming increasingly clear the world was about to face an unprecedented threat. By Feb. 24, the day Cardy gave his grim presentation to New Brunswick Tories, Tam had stopped sounding quite as calm. “These signs are concerning,” she told reporters, “and they mean that the window of opportunity for containment, that is for stopping the global spread of the virus, is closing.”
Canada had failed to take the steps that might have stopped the virus from getting a foothold. COVID-19 was about to put the country through its worst crisis since the Second World War. Some countries saw the warning signs. Why didn’t we?
***
There is a hint of an answer in PHAC’s first public statement about the virus. On Jan. 6, when a spokesperson assured Canadians they were protected by a Canadian centre that describes itself as “an indispensable source of early warning for potential public health threats worldwide including chemical, biological, radiological and nuclear,” he was describing the Global Public Health Intelligence Network (GPHIN). But since 2019, GPHIN had not been functioning as it once did. Tam seems to have been flying blind.
GPHIN was established in 1997. In its heyday, it employed analysts and experts based in Ottawa and around the world, who scanned media, stock markets, open-source data and social networks for signs of health threats, acting almost like a high-tech health CSIS, repurposing information to find infected needles in haystacks. They shared those updates with health experts around the world. The system is still functioning, but Grant Robertson reported in the Globe and Mail in July 2020 that it had been downgraded by officials in 2018, who wanted it to focus on more relevant domestic issues, such as the health risks of vaping. Hajdu announced an independent review in February 2021, a tacit acknowledgement that it was broken.
Decision-makers had been warned. In 2018, PHAC epidemiologist Abla Mawudeku emailed international colleagues in despair. “I would like to let you know that, sadly, we have not been successful in convincing management of the critical value and role of GPHIN within and outside of Canada, and the indispensable relationship with the WHO,” she said in an email later obtained by the Globe. International experts, too, lamented the agency’s decline. “GPHIN has been a pioneer in what was, at that time, a totally barren field,” Philippe Barboza, a manager of the WHO’s Health Emergencies Programme, wrote in an email to Canadian epidemiologists. “I cannot understand that this is not recognized.”
GPHIN’s parent organization—the public health agency—had serious problems of its own. An internal audit made public in January 2021 is blunt: PHAC wasn’t ready for a pandemic. “The agency did not have the breadth and depth of human resources required to support an emergency response of this never-seen-before magnitude, complexity and duration,” auditors found, after interviewing “52 key informants.”
“Management noted multiple capacity and skills gaps across the agency,” the audit continued. “Primarily, most noted limited public health expertise, including epidemiologists, psychologists, behavioural scientists and physicians at senior levels.” As we faced the biggest pandemic in a century, the Public Health Agency of Canada didn’t have enough doctors.
When COVID hit Canada, dedicated staffers were working brutal hours, called on to acquire PPE, to help the provinces and territories get ready for contact tracing and set up quarantine sites, to help prepare prisons. But “there was a limited number of quarantine officers within the agency and it was a difficult position to staff quickly because it requires specific education and training,” the audit said. PHAC did what it could to fill the gap, but when Trudeau eventually closed the land borders and called Canadians home in March, there appear not to have been enough people to handle the traffic.
Tam was getting bad advice. “Her office noted that she often received information in the wrong format, with inaccuracies, or in an inappropriate ‘voice’ needed to convey information to a particular audience,” the audit reported. “The modelling information, critical to the public face of the response, and the foundation for strategic planning, was mentioned as being problematic in its initial stages, because of the lack of a coordinated or strategic approach to the work.”
The problems seem to go back to 2014, when then-health minister Rona Ambrose reorganized the agency, which was created after the SARS outbreak, with the chief public health officer in charge. The reorganization, introduced as part of an omnibus bill, demoted the chief public health officer—a doctor—and established a new head of the agency: the president, a civil servant. Ambrose said in the Commons that the move was “aimed at strengthening both its internal management and public health capacity.”
It appears not to have done so. Epidemiologist Michael Garner, who left the agency in 2019 as a senior science adviser, said the reorganization integrated the agency into the general bureaucracy, bringing in people from other departments without the specialized skills a public health agency needs. Garner left in 2019 to follow his ambition to become a priest; he now ministers to souls at the St. Thomas the Apostle Anglican Church in Ottawa, where he has found himself advising the bishopric on how to safely continue pastoral work during a pandemic.
When he left PHAC, he was lead researcher on a team focused on emerging infectious disease risks. He was glad to get out of there. “With the way—under the Harper government—science was sort of frowned upon, with the reorganization, and with the rewriting of this Public Health Agency of Canada Act where the [chief public health officer] was demoted and a president who was a bureaucrat was put in charge, our team was pushed to the side,” he said. His friends who remain at PHAC “have worked tirelessly over these nine months at great costs to their families, to their own health. So I think they’ve done a great job. But I think Canada has done a very poor job.”
Carolyn Bennett, a family doctor before she became a Liberal MP, had established the agency while serving as minister of state for public health under Paul Martin. She opposed Ambrose’s reorganization. “It was [supposed] to be an agency head with the expertise that could go downtown and get the money and be able to set the priorities,” she told the Globe and Mail in 2014. “Anybody I’ve talked to about [the proposed changes] in the public health community has the same two words: bad news.”
But the Trudeau government did not reverse the changes. Garner blames the Harper government for breaking PHAC, and the Trudeau government for failing to fix it.
Bennett had set up the agency so the person in Tam’s job could speak independently. Harper’s government didn’t like being contradicted by scientists, so they changed it. “There was a very clear decision to make a chief public health officer the head of the organization, where that person would have all of the power and that person was empowered to speak to the public,” said Garner. By restructuring PHAC, the government had allowed the scientists to be subsumed by the culture of the amorphous Ottawa bureaucratic blob, which is not always entirely task-oriented.
On Jan. 27, when Tam testified before a Commons committee, telling them it was not necessary to quarantine travellers returning from Wuhan, she was introduced by Tina Namiesniowski, her boss at PHAC, a civil servant with stints over the years at the Privy Council Office, the Treasury Board, National Defence and Canadian Heritage. Namiesniowski, who resigned around the time the audit was written, said Tam was acting “to ensure an authoritative voice to all Canadians during a public health event, which is essential.” The audit said they worked well together, “standing constantly behind one another, supporting each other and sharing the pressure together.”
It seems fair to wonder if they were too close. Was the government listening to Tam, or was it just using her, as Namiesniowski said, as an “authoritative voice” for a government that wanted to project calm?
On March 5, the WHO’s Tedros was blunt: “This epidemic is a threat for every country, rich and poor, and as we have said before, even the high-income countries should expect surprises.” Five days later, in Ottawa, in an incident described by my colleague Paul Wells in an article for this magazine, a reporter coughed into her balled-up fist at a news conference; Hajdu reminded everyone that it’s safest to cough into one’s elbow and to stand two metres apart, which nobody in the Commons lobby was doing. “But I will also remind Canadians that right now the risk is low,” she added, twice.
Unlike Dr. Anthony Fauci, who often gave interviews contradicting the catastrophically dangerous COVID-19 advice of U.S. President Donald Trump, Tam’s comments have been in lockstep with her political masters. That close alignment of messages may be because the Liberals seemed to take Tam’s advice, unlike Trump, whose former adviser expressed a desire to behead Fauci. But it may also be because the Liberals were using her as a spokesdoctor.
“Does Theresa Tam have complete licence to call it exactly as she sees it?” asks Steven Lewis, an adjunct professor of health policy at Simon Fraser University. “If the answer is yes, then arguably Theresa Tam was overly optimistic about how this was going to go. The messaging wasn’t sufficiently clear and there was just too much wiggle room.”
Lewis thinks she does not have licence, that her role is to stay onside with the government she serves. But the public statements Tam was giving weren’t that different from those of Fauci. They were both likely worried about looking like Chicken Little—a bad position for a public health leader. On Feb. 13, health reporter Helen Branswell, who was worried by COVID’s progress, pressed Fauci on why he wasn’t raising the alarm. Fauci asked how it would look if he was wrong. “I’m telling you we’ve got a really, really big risk of getting completely wiped out, and then nothing happens? Your credibility is gone.”

Playgrounds sat idle during the height of the lockdowns; in this Toronto park on March 26, 2020, fun was off limits (Lorne Bridgman)
***
I started to worry about the virus on March 11, when I listened to a webinar by Dr. David Fisman, an epidemiologist at the University of Toronto. I was in Punta Gorda, Fla., at the time, fixing up an old sailboat I hoped to sail to the Bahamas. Sitting on my boat, with bad marina WiFi, I managed to download the Fisman webinar and soon found myself sweating, and not from the heat. Fisman had just revealed modelling that projected up to 70 per cent of Canadians could be infected unless we implemented measures to prevent the virus spreading.
Fisman began by explaining to his audience—the Canadian Society of Association Executives—that he was a “little nervous about what I’m going to bump into in the hospital over the coming weeks.” COVID-19 is a recombinant virus, Fisman explained, which means that it evolved while jumping between animal species before moving on to humans. It is “made up of different viral strains that sort of got glommed together into a recombined virus that turns out to be very virulent,” he said. “It makes people quite sick, but [it’s] also quite transmissible, so that each old case makes two new cases or three new cases before they get better.”
That means it can spread exponentially. That was the part that scared me—the terrible silent spread, leading to a sudden wave of illness that could overwhelm hospitals, as was happening in Italy.
“When we have epidemics presenting with deaths, what that means is it’s an old epidemic, because it takes people a while to get sick enough to die,” Fisman explained. “So, we have a bit of a heuristic. If you see two deaths, and we think case fatality is two per cent, those two deaths represent 100 cases, and they represent 100 cases from two weeks ago. So those 100 cases with a reproduction number of two means 200 cases the next week . . . So you’ve got a minimum of 700 cases in your population by the time you see two deaths.”
I emailed Fisman and asked him for an interview for a story. We spoke on the phone on March 12, the same day Ontario Premier Doug Ford told families they should not cancel their March break plans: “Go away, enjoy yourself and have a good time.” I had come to believe Canadians needed to be frightened.
Fisman agreed. “Everyone should be very scared.” He was convinced that governments were acting too slowly, that leaders were failing to grasp the situation. “We have a choice here right now, which is we can be Hong Kong or we can be Italy,” he said. “We get to choose one or the other. We don’t get to choose the status quo. And the difficulty for the politicians is that if you shut things down now and it’s quiet and you achieve what you wanted to achieve, which is nothing happens, then you’re going to be excoriated for overreacting. You achieved what you set out to achieve, which is we didn’t kind of go through what the Italians went through and that’s why we did that. And then people are going to say, bastards! You cancelled the NHL season. And then my restaurant got no customers for a month. You’ve ruined me!”
Fisman was beginning to be a target. The day before I spoke to him, he did an interview with the National Post in which he discussed his model. “The rage that came at me, it’s really something I’ve never experienced before,” he told me at the time. (He has experienced much worse since.) “I think people are scared and there’s a separate grieving thing going on here as well, where there’s denial and anger and all those emotions.”
Before we finished the interview, I decided to ask for Fisman’s advice about my own situation. I had been in Florida for a few months, where boardwalks remained busy and the waterfront bars were still packed with sunseekers drinking pitchers of Bud Light and listening to dad bands. Even after the NBA suddenly cancelled its games, the people I talked to in Florida were unconcerned, dismissing the virus as media nonsense. The Gulf Coast of Florida is Trump country, and the president was telling people not to worry. On March 10, he famously promised it “would go away.” I imagined the virus spreading, silently, and started hiding on my boat, trying to minimize my exposure.

Florida’s beaches and waterfront bars in mid-March 2020 remained packed with people unconcerned about media reports of the virus (Saul Martinez/The New York Times/Redux)
I had started to worry about what would happen if I got the virus. How would I get medical care? How would I get home? I apologized for using an interview subject for medical advice, and asked Fisman what I should do. He pointed out that only three places in the entire state of Florida were doing COVID testing. And there are a lot of seniors in Florida. “If I were in your boots, I’d probably come on back.”
I moved my boat to storage, rented a car and made the long drive north, 2,400 km, from palm trees to snow, past many golden arches and Exxons, up Florida, through Georgia and the Carolinas, around Washington, D.C., then up through Pennsylvania and New York state. I listened to Albert Camus’s 1947 novel The Plague as I drove. I wore disposable gloves when I filled the gas tank. I avoided restaurants and bathrooms. When it got cold, in upstate New York, I parked at the edge of a truck stop and changed my clothes in the darkness of the parking lot.
At first, there were a lot of RVs, trucks hauling boat trailers. The parking lots in the malls and roadside barbecue joints were full. The further north I got, the more seriously people seemed to be taking the virus. In Pennsylvania and New York state, the digital highway signs—the kind that usually warn of congestion ahead—all had warnings about the virus.
I was part of an enormous movement of Canadians home—the flight of the snowbirds. On March 16, Trudeau had announced that Canada was finally taking dramatic action, closing its borders to most foreigners. “If you’re abroad, it’s time for you to come home,” he said.
About a million Canadians returned that week—in planes from airports around the world, and a huge wave from trailer parks and retirement villages in Florida and other U.S. states. It was an unprecedented influx.
Trudeau had called us home, but somehow there was no plan to safely handle us. The airports were a mess. Travellers were jammed together in waiting areas. Masks were still not recommended, and few were wearing them, a shocking contrast for Canadians returning from Asia, where everyone was masked. Scott Grant and his wife flew from Thailand to Vancouver on an Air Canada flight, on their way back to Saskatchewan after a long holiday. When they stopped in Hong Kong, they had their temperatures checked repeatedly with thermal sensors. On the flight, everyone was masked. When they arrived in Vancouver and left the plane, the passengers at the next gate appeared to be coming from a different world. “We pull up beside a flight from London, and not one person from the flight got off with a mask on,” he said.
Not for the last time in the pandemic, there was a gap between the official version and reality. On March 13, Public Safety Minister Bill Blair tweeted: “We have enhanced screening measures in place at all international airports, as well as land/rail/marine ports of entry. We are taking the necessary steps to ensure that Canadians are safe in the face of COVID-19.” But travellers were quick to respond on social media with stories and pictures showing those measures weren’t being implemented. Glen Canning, a Nova Scotian resident in Toronto, shared pictures of a jammed terminal at Toronto’s Pearson International Airport: “I’ve been in the Canada customs line at Pearson for over an hour along with hundreds of people. Six agents on duty, zero screening, no masks, no sanitizer in site. This is as unsafe as it can get.”
Tam was trying to get the message out. “We are asking that all travellers that come back self-isolate,” she said to reporters on March 15. “This is a voluntary self-isolation. It is impossible to keep tabs on every single traveller who comes in. This is a social phenomenon. This is a societal response and everybody must take that responsibility. Public Health is going to do what it can.”
But travellers weren’t consistently being advised to self-isolate everywhere. A passenger freshly landed in Vancouver after a flight from Mexico sent me a cellphone picture of the pamphlet he had received, which did not mention self-isolating.
It remains a mystery why the measures announced by Trudeau and Bill Blair were not being implemented. I sent questions to Public Safety and the PMO last March, which they have yet to answer. Off the record, officials will only say they were overwhelmed.
***
In Moncton, N.B., Roxann Guerrette, Cardy and Smith were solving the problem. Guerrette was then working remotely for Distributed Bio Inc., a San Francisco pharmaceutical start-up researching a universal flu vaccine. Both the company and Guerrette were featured in Pandemic: How to Prevent an Outbreak, a Netflix series released in January, just as COVID was about to go global.
On Jan. 25, Distributed Bio started working to “engineer a panel of anti-SARS antibodies” to treat what later became known as COVID. Guerrette, an Acadian from the northern New Brunswick community of Sainte-Anne-de-Madawaska, became aware from online conversations with colleagues in Europe that the virus could be a dire threat. “I just knew this would be a pandemic before the government started to act upon it,” she said.
Guerrette and Cardy, the N.B. education minister, had gotten to know each other when she was president of the university’s student union. She was impressed by his pro-science approach and in particular by a bill he had tried to get passed requiring mandatory vaccination for all New Brunswick schoolchildren, a measure narrowly defeated in a free vote in the legislature.
As he and Smith worked on their report for the premier in February, Cardy leaned on Guerrette for help understanding some of the scientific concepts. They shared a sense that Canada was failing to get ready. “Scientists have known for a while that this could happen, that there could be a virus that would take over the planet and we’d have to find strategies to mitigate it,” said Guerrette. “We had the Spanish flu. It’s something that can happen again. And Dominic Cardy kinda knew that this could happen again and the best way was to act fast.”
Guerrette sent Cardy COVID-control protocols she had received from a colleague in Israel. She organized a billboard campaign to encourage people to wear masks, which she considered protective, while Tam was still advising people against them. She convinced her boss, scientist Jacob Glanville, to do a video warning New Brunswickers to practise physical distancing, which she and Smith shared on social media. She raised money to get protective equipment for health-care workers.
When Trudeau called people home, a dedicated group of New Brunswickers realized travellers would be bringing COVID with them. Léger, the chief of staff to the premier, said the province knew it had to tell the convoys of returning travellers coming over the border from Maine to isolate. They needed to be instructed to go straight home, without stopping to buy groceries or visit their relatives, but the Canada Border Services Agency wasn’t going to give the instructions. “Their job was to let people in Canada,” said Léger. “Once they are in Canada, that’s another ball game. So they were travelling to Canada, but as soon as they cross over, they’re already home.”
The province put game wardens on the roads in makeshift roadblocks to give health advice to the returning snowbirds. Civil servants weren’t sure. “Are you sure you want to do that?” Léger recalls some asking him. “ ‘Pretty much.’ The premier was absolutely steadfast.”
Cardy and Guerrette tackled the problem at the Moncton airport. He wired her $250. She went to the Canadian Tire in Dieppe, N.B., where she bought tape, 20-litre jugs of water and bottles of bleach to mix to make disinfectant. They printed pamphlets advising people to self-isolate. She went to the airport, said she was acting on Cardy’s authority, and started organizing the arrivals area, getting hand sanitizer for the airport workers and putting tape on the ground to enforce social distancing, directing people over whom she had no authority in both official languages.
The returning travellers needed to be told what to do, she said. “It was a bit of a shock for them and they couldn’t understand that they couldn’t stop at McDonald’s to get a burger on their way home. And we literally needed to put tape on the floor because people wouldn’t listen to the six-foot-distance rule.”
Guerrette got some blowback. She endured social media attacks that still leave her bruised a year later and a country away. She is now working for a biotech company in Boston. “She was personally brave and ready to stand up and put her credibility on the line,” Cardy said. “She didn’t make herself any friends during that period, but she saved many lives.”
Cardy, too, made enemies. Parents complained when he ordered students who had been out of the country on March break to stay home from school for 14 days. Public health officials in New Brunswick opposed the measure, and Dr. Rama Nair, a professor of epidemiology at the University of Ottawa, told the CBC he was being too cautious. Dr. Chris Goodyear, then the president of the New Brunswick Medical Society, said physicians did not believe the measure was rooted in evidence-based public health policy.
Looking back, it seems strange. Tam was wrong, as were many public health experts. On March 11, Steven J. Hoffman, a professor at York University and director of the WHO Collaborating Centre on Global Governance of Antimicrobial Resistance, praised Canada’s measured response on a TVO panel show. “It really highlights the decision that many governments, fortunately not Canada, but many governments out there when they are imposing travel restrictions,” he said. “We see many countries around the world are overreacting to this threat. The overreaction can actually cause more harm than the virus itself. For example, there are 180 million children in China who are not at school. . . ”
Because of the stringent measures China took, that country has been largely free of the virus since March.
In January, Chinese officials were urging citizens to wear masks, part of the successful national measures that suppressed the virus. Tam didn’t advise Canadians to mask up until April, a few days after the CDC changed its policy. Until then, the research was unclear. Both Tam and the CDC were wrong. And because they didn’t advise wearing masks, warned against the risks, in fact, people got infected and died. But they didn’t know they were wrong. Perhaps they couldn’t have known.
It is difficult to remember now all the things we didn’t know then. On March 15, I was thinking about writing an article calling for the cancellation of St. Patrick’s Day, or at least the part most people like about it: drinking beer in bars and listening to Irish music. I emailed Fisman to ask his opinion. I noted the stories from Italy about young people partying and spreading the disease. “Also,” I added, “South Korean data show high rates of asymptomatic young people.”
“God bless the South Koreans,” he replied. But his answer to my question was careful. “They’re delineating the true epi of this disease with the massive testing. Re St. Paddy’s day . . . I have enough trouble in my life without saying ‘close the bars on St. Paddy’s’ in Maclean’s. But one can easily see how bars would be good for spread.”
He, too, was grappling with a strange new world. It should have been obvious that we needed to close bars, but we were both struggling to come to that conclusion. So were our leaders.
On March 13, Dr. Mike Ryan, an Irish doctor who has spent his career doing emergency medicine in the most difficult places in the world, discussed the necessary mindset during a WHO news conference. “The lessons I’ve learned after so many Ebola outbreaks in my career are: Be fast. Have no regrets. You must be the first mover. The virus will always get you if you don’t move quickly, and you need to be prepared. One of the great things in emergency response—and anyone who’s involved in emergency response will know this—if you need to be right before you move, you will never win.
“Speed trumps perfection, and the problem in society we have at the moment is everyone is afraid of making a mistake, everyone is afraid of the consequence of error. But the greatest error is not to move, the greatest error is to be paralyzed by the fear of failure.”
***
Looking back at the pictures Glen Canning took at Pearson airport, it is strange to see so many people without masks crammed together. There is no way of knowing how many people got infected in the crowded lines at Pearson, but likely a lot. And some of them likely died. A Statistics Canada report from April 2020 found a quarter of COVID cases were directly linked to travel.

Toronto’s Pearson International Airport, on March 14, 2020, was packed with crowds of unmasked people as Canadians returned home (Glen Canning)
A lot of highly educated, dedicated and motivated people failed to sound the alarm, and to heed it when others did.
It made me think of the disaster in Aberfan, a Welsh coal-mining town, where mine waste had been piled on top of streams on the hillside above the town. After a night of heavy rain, the pile of debris slid down the hill, where it crushed a school, killing 109 children and five teachers. The tragedy was dramatized in an episode of The Crown, I later learned. But the part of the narrative that is less well-known is that the local council had complained for decades about the slag heaps, which repeatedly flooded parts of the village with dirty water. In 1963, an engineer warned the National Coal Board: “The slurry is so fluid and the gradient so steep that it could not possibly stay in position in the wintertime or during periods of heavy rain.”
But officials at the coal board, who were ultimately found responsible at a public inquiry, ignored the warnings, and so on Oct. 21, 1966, miners who started their day digging coal finished it digging the remains of their children out of what had once been a school.
The sociologist Barry Turner, in a 1976 study of man-made disasters, including Aberfan, found that organizations often have a “tendency to minimize emergent dangers.” Part of the problem is that officials reflexively discount the views of non-experts, like the villagers who warned the coal waste was ready to slide.
The people who see the danger are, like the mythical Cassandra who warned the Trojans there were Greek soldiers in the wooden horse, ignored because they are not part of the group in charge. Experts often respond with a “high-handed or dismissive response,” Turner wrote. Warnings from outsiders are “fobbed off with ambiguous or misleading statements, or subjected to public relations exercises, because it was automatically assumed that the organizations knew better than outsiders about the hazards of the situations with which they were dealing.”
I emailed that quote to Cardy when I came across it.
“I’m framing that,” he replied.
***

Dr. Simon Demers-Marcil, an ICU physician in Calgary, calls a family to tell them a loved one has died of COVID-19 (Leah Hennel/AHS)
Chapter Two: Canada’s strongest bubble
‘What experience and history teach is this—that people and governments never have learned anything from history’—Hegel, Philosophy of History
On March 29, 1919, in the middle of a pandemic that had started during a world war, the Montreal Canadiens faced the Seattle Metropolitans in the Stanley Cup final. It didn’t look good for the Canadiens at the beginning of the third period in the fifth game. Les Glorieux had to win to have a shot at the cup, but they were trailing 3-0, and their best defenceman, scrappy Joe Hall, a man who once said he played so rough he was “giving a dog a bad name,” was too ill to finish the first period. They somehow rallied, led by Édouard “Newsy” Lalonde, who scored two goals to tie the game, before Jack McDonald put them up 4-3 in overtime. It was a thrilling conclusion to what the Vancouver Sun called “one of the best and fastest exhibitions of hockey ever seen here.”
The stage was set for Game Six, but it was not to be. Five Canadiens were in the hospital with the flu. Hall died a week later. The Habs, without enough men, forfeited, but the Seattle side wouldn’t take the victory, and eventually this was engraved on the cup: 1919, Montreal Canadiens, Seattle Metropolitans, Series Not Completed.
Hall was one of about 50,000 Canadians to perish from the so-called Spanish flu, at a time when there were only 8.8 million Canadians. The flu’s impact, like COVID’s, was greatest on the vulnerable, people who couldn’t avoid infection, or count on proper care once infected. It cut a horrible swath through Indigenous communities, who were vulnerable thanks in part to widespread tuberculosis and federal policies that left them malnourished and ill cared for. And its second wave was worse. In 1918, the Canadian government repeatedly seeded the flu by dispersing infected soldiers around the country without considering the consequences. Vincent Massey, who would later become governor general, wrote a scathing report for prime minister Robert Borden, laying out the federal failure: the government, Massey wrote, “could have given specific directions and ensured that a uniform, coordinated plan was followed.”
A hundred years later, as Canada inched toward the second wave of another pandemic, you could say much the same. Ottawa moved quickly last spring to provide income supports, hatching the CERB program within weeks of the country going into lockdown and providing up to $2,000 a month for those deprived of work. Other programs followed for businesses and individuals. They were all criticized for various reasons, but the money kept the economy moving, preventing terrible deprivations.
What the federal government didn’t do is impose a coordinated response on the provinces, as it might have done if it had invoked the Emergencies Act. In the ensuing months, Tam and Trudeau repeatedly called for provinces to take stronger action. The premiers of Quebec, Ontario, Manitoba, Saskatchewan and Alberta mostly ignored those warnings, as well as the lessons of history, and the failure to suppress the outbreaks belongs to them.
In late August, as Canadians visited gyms, bars, restaurants and shops, and schools geared up to reopen, the warnings from health experts grew more urgent. So did their calls for investing in rapid testing and contact tracing. By Jan. 15, without adequate measures in place, the second wave had crested. There were an average of 9,600 new cases a day across the country, about 1,000 of them in Toronto. It has been an ordeal, said nurse Kathryn Rego, who helped care for Canada’s first COVID patient in that city last March. “There was never a thought in my mind that we’d be in lockdowns a year later,” she said, “still fighting this thing and seeing the strain on the hospitals and the strain on the staff and just the burnout.”
On the other side of the world, Melbourne, Australia, a city of five million, was heading into its tenth day with no new cases. Steven Lewis, the health policy professor at Simon Fraser University, has spent the pandemic in Melbourne and thinks Australia did better because its leaders were bolder. Lewis, a long-time senior health policy professional from Saskatchewan, found himself in Australia when his partner got a job there. He has been functioning as “head of domestic affairs” for his family, spending his spare time keeping a close eye on pandemic management in both countries. Australian leaders, he found, did not count on everyone taking responsibility for their actions, the approach taken by Canadian authorities early on.
“The first obligation is to have a clear policy, and the messaging [in Canada] has been, for the most part, extremely ambiguous and always leaves a little wiggle room,” said Lewis. “So you get the chief medical officer saying, ‘We really would discourage people from having mass gatherings’ or ‘You really should restrict unnecessary travel.’ Well, what do you mean by that? Are we allowed to travel or not? And who defines unnecessary?”
Even some helping to make policy interpreted the advice loosely. Last November, Dominique Baker, surely the first acting manager at the Public Health Agency of Canada’s Office of Border Health Services to make headlines, took an all-expenses-paid trip from Air Canada to Montego Bay, Jamaica, to stay at an elite resort. She gushed about the luxurious experience on her style and beauty website, and posted about it on Instagram. After the trip came to light, she was publicly criticized by Iain Stewart, who had replaced Tina Namiesniowski as the boss at PHAC. Baker expressed regret and, before long, announced she was leaving the government to pursue her dream of being a full-time social media influencer.
Baker comes across as a sympathetic person on her style website, and her delight at riding a horse on the beach in beautiful Montego Bay is infectious. But she was travelling in the thick of the second wave, for non-essential purposes, while she had a crucial role in the white-knuckle business of managing travel during a pandemic. She was not the most senior Canadian official to abandon her post to sneak away to a sun spot: Rod Phillips, the Ontario finance minister, decided to spend Christmas on posh St. Barts. Before he left, he recorded a series of holiday greetings for scheduled posting online that suggested he was still in chilly Ajax, Ont. More ill-advised jaunts came to light in the first grim days of 2021: Alberta MLAs in Hawaii and Mexico, the Niagara Health CEO Tom Stewart in the Dominican Republic. A number of those people lost their jobs. Some Canadian leaders in charge of protecting the health of the country obviously had other things on their minds.
From the beginning, Australia responded more decisively, shutting down travel from affected areas and enforcing measures meant to control the spread of the virus, with fines and spot checks when necessary. The state government in Victoria implemented a hotel quarantine order for out-of-country arrivals in March 2020, 11 months before Canada took a similar step.
The aggressive action worked in the first wave: Australia had 4,559 cases at the end of March while Canada had 8,589—23 per cent less per capita. That difference only grew. Tough action all but eliminated the virus from Australia within a month, while cases in Canada kept climbing. Australia had the pandemic under control until June (the start of its winter), when sloppy private security guards at a quarantine hotel got infected, leading to hundreds of cases. The virus spread through asymptomatic people attending family gatherings. The second wave was getting out of hand, relatively speaking, until the state government brought in a tough 111-day lockdown in July, with most people confined to their homes—quite a feat in Melbourne, a city of five million. By August, residents had to observe a curfew and stay within five kilometres of their homes, which they were only allowed to leave for essential purposes or for an hour or two of outdoor exercise. Gyms and schools were closed. Restaurants were only allowed contactless delivery and takeout.
“You can’t say, well, because 80 per cent of the population believes the way we do, we’re going to be successful at pandemic control,” said Lewis. Everybody has to be ordered to comply, or the measures won’t work. Australian politicians were prepared to take dramatic steps. Prime Minister Scott Morrison mused about making vaccination mandatory (he later backtracked). Police in the state of Victoria issued more than 20,000 fines for COVID violations, which helped shut down transmission, although human rights groups complained the penalties were applied inconsistently, targeting more minorities. The measures were harsh and enforcement wasn’t perfect, but they worked.

In contrast to Florida’s bustling shores, this empty beach in Sydney, Australia, shows how seriously the country took lockdown (James Gourley/Getty Images)
That took political leadership. “You have an enormous political dimension to what is essentially a scientific and technical problem to solve,” said Lewis. The Australians found the political will. Canadian leaders didn’t. We have lost more than 22,000 people to COVID. Australia has lost 909.
Our disorganization and lack of political will means we got sicker and are poorer. “We’re paying a bigger economic price because we didn’t do it,” said Lewis. “It’s not that Australia chose to pay a higher economic and ancillary-health-concerns price in order to do this. They figured if we do it hard and we sustain it and we stick to our goals . . . until it is very clear we can reopen in the long run, we will be better off, not just health-wise, which is incontrovertible, but also economically.”
Crucially, Australia broke with the advice of the WHO early on, imposing travel restrictions while Canada was still following advice from a body that critics think was unduly influenced by China. Australian leaders were not afraid to act quickly and decisively. Canada was always behind the play. “You don’t even know what the puck is at the beginning, let alone where it’s going,” said Lewis. “So to anticipate is critically important and we’ve chased the puck. Canada’s still chasing. They still wait before they move to another level of lockdown.”
***
In July, I moved home to Nova Scotia after 15 years in Ottawa’s ByWard Market, a lively, pedestrian-friendly neighbourhood full of shops and restaurants that was suddenly empty and charmless in March. I was alone in my apartment, working on stories about the shooting rampage in Nova Scotia, struggling psychologically with the tragedy, frustrated at the distance, so I decided to move back.
The Atlantic provinces had restricted interprovincial travel starting in March, requiring most travellers entering the region to spend 14 days self-isolating, and discouraging internal travel during outbreaks. (“Stay the blazes home,” in the words of Stephen McNeil, then Nova Scotia’s premier.) But after a two-week quarantine in a seaside cottage, I was delighted to roam freely in a jurisdiction where everyone wore masks without complaint in the supermarket although there was virtually no infection—two active cases in the middle of July. It felt like a place apart, a land without COVID. Restaurants and bars were full. Real estate agents were overwhelmed with business from Upper Canadians seeking a seaside escape.
The dark side, if you could call it that, was a certain nosiness—part of the social cohesion that kept the region safe. One day, I stopped by the side of the road on St. Margarets Bay to look at an old fish shed—a shingled building on the rocks at the water’s edge. I walked across a lawn and asked the shed’s owner if she would mind if I had a look, and mentioned I had recently moved home from Ontario. She was friendly, and told me that was no problem. “But have you registered?” she asked. I had wandered into a campground, which she owned. Everyone leaving or entering the campground was required, by provincial order, to register. I could look at her shed after I registered, she said.
I agreed and followed her to the office, where I wrote down my name and number. She then asked for proof I had self-isolated, adding that many people were dishonest about the quarantine. She wanted to know I wasn’t fibbing. I declined to show her my travel documents, which I was not required to do, and left, both of us exchanging polite farewells through gritted teeth.
I didn’t like being quizzed by a self-appointed health inspector, but I am sure this kind of vigilance is part of why Atlantic Canada was able to avoid the worst of the pandemic. In Prince Edward Island, some cars with out-of-province plates were vandalized by local quarantine enthusiasts. Cortland Cronk, a New Brunswick software consultant and marijuana nutrients supplier, moved out of the province after he travelled for work, was blamed for an outbreak back home, and criticized online. Atlantic observers were skeptical of his narrative but he received solicitous treatment from the New York Times, which described pandemic shaming as “a worsening civic problem.”
Premier Stephen McNeil, who left office in February after presiding effectively over the pandemic, told me Atlantic nosiness may have been part of the success. “They would let us know if you weren’t isolating,” he said in an interview during his last week in the job. “But on the flip side, we had to tell people just because someone’s here with an [out-of-province] licence plate doesn’t mean they haven’t isolated. It doesn’t mean they don’t have a right to be here.”
“We tried to frame that in a positive way, communities caring for each other, supporting people,” said Robert Strang, Nova Scotia’s chief medical officer of health. “We’re not stressing the compliance if you will, but a bit of that ‘I’d better be careful because somebody may be watching me’ is probably helpful as well.”
McNeil said he and Strang acted decisively in part because they knew the limits of Nova Scotia’s health system. “I was terrified of what was going to happen to our health-care system and to Nova Scotians when it came in,” he said. “That’s why at the front end we were so aggressive.”
The provinces west of Rivière-du-Loup, Que., even in the tightest lockdown in the spring, mostly declined to institute travel restrictions, arguing that the Constitution allows for free movement within the federation. A November study in Nature Human Behavior that analyzed responses around the world found travel restrictions were among the most effective measures globally in curbing the pandemic in March and April 2020, but Canadian politicians mostly declined to impose them. They faced pushback from voters who bridled at the prospect of being kept away from their cottages, which, after all, they own. The virus, which doesn’t care about our Constitution or the requirements of second-home maintenance, took advantage. The district that encompasses Simcoe-Muskoka, the beautiful cottage country north of Toronto (population 550,000), suffered 189 deaths, compared with Nova Scotia (population 970,000), which lost just 65 people, almost all of them at one large long-term care home.
While Ford was telling Ontarians to go away and enjoy themselves on March break, McNeil was warning people they would have to isolate on their return. Nova Scotia and its Atlantic neighbours did a hard shutdown in the spring of 2020. “My background before I came into this office, I was self-employed,” said McNeil. “I knew I was taking four months’ income from people. I was closing them down.” He didn’t want to do it, but is sure it was the right call. “That’s not an easy decision to make, but it was absolutely the right decision. We couldn’t, in the front end, say, ‘We’re going to leave you half open.’ We had to close it to understand it.”
***
In November, it looked briefly as if Nova Scotia was in for a second wave. Cases started rising, as they were across Canada. McNeil and Strang had evidence the virus was spreading through asymptomatic customers in Halifax bars and restaurants, so they prepared to tighten restrictions.

As much of Canada descended into a second wave in late 2020, Halifax gym goers were able to continue group fitness classes (Tim Krochak/Bloomberg/Getty Images)
Restaurant owners had a better idea. Gordon Stewart, executive director of the Restaurant Association of Nova Scotia, asked the province to shut them all down.
On Nov. 24, with Nova Scotia reporting 37 new cases of COVID, the province agreed to the industry’s request. Instead of tightening the rules, they ordered indoor dining shut. “We wanted to stay open,” Stewart told me. “The difficulty was, if you shut down and reopen, shut down and reopen, that can be very expensive. It’s expensive being closed, but it’s not as bad as being closed, reopened, closed, which has happened to many parts of Canada, and other parts of the United States and Europe.”
The restaurants and bars lost their busiest season—they remained shut through the holidays—but when they reopened in January, they reopened for good. “We knew if we locked down and made it tight, then that number would go back down,” said Stewart. “And that’s exactly what happened to us in Nova Scotia.”
Former health minister Jane Philpott thinks it is better for businesses if governments lock down hard enough to eliminate the virus. “I think many people would say, yeah, we would have rather been entirely shut down for a month or two,” she said in a recent conversation. “And not have the torture we’ve had over the winter of this long drip, drip, drip of economic challenges.”
Arguments about the social and economic costs of lockdowns really only apply to lockdowns that fail. Lockdowns that work are ultimately good for the economy. As it turns out, in Nova Scotia, according to Stewart, restaurant receipts in January 2021 were at about the same level as January 2020, before the pandemic hit. The province’s unemployment rate is lower than Alberta’s for the first time in memory.

Eight nurses and two respiratory therapists work together to prone a patient at Peter Lougheed Centre, Calgary, on Jan. 13, 2021. (Heather Patterson)
***
There was a moment in the early fall, before the second wave, when provincial governments in most of Canada could have responded more decisively and shut down the virus. Canadians were flocking to malls and gyms and restaurants even as cases were starting to rise. University epidemiologists urged leaders to act. Instead, governments took half measures.
The second wave, like the first, arguably started in Quebec. In September, after a karaoke party at Bar Kirouac in Quebec City led to at least 72 cases, the province responded not by shutting bars but by banning karaoke, which led to angry complaints from bar owners. Quebec Premier François Legault waited until midway through December, when the health-care system was under strain, to take the harsh steps needed to slow the spread.
The Prairie provinces had avoided high case counts in the pandemic’s first wave. Their conservative premiers were among the first to ease restrictions in the spring and summer, and they were reluctant to close again later. Manitoba, which often had no new daily cases in May and June, saw rapid spread start in August, settle briefly, then take off in September. It has had Canada’s highest COVID fatality and hospital rates outside of Quebec in spring. Premier Brian Pallister made an emotional presentation to Manitobans in December, urging them to follow the rules. “So I’m the guy that has to tell you to stay apart at Christmas and in the holiday season you celebrate . . . where you share memories and build memories,” he said, his voice breaking. “I’m that guy. I’m the guy who’s stealing Christmas to keep you safe because you need to do this now.”
In Saskatchewan, Premier Scott Moe cried foul when Trudeau called for provinces to tighten up on Nov. 10. “We can keep our economy open and people working by following sound practices that reduce the spread of COVID-19,” he said. There were 127 new cases that day. A month later, averaging 260 new cases a day, Moe brought in tighter rules. Saskatchewan would have been better off if he had heeded Trudeau’s warning.
British Columbia did better than all but the Atlantic provinces in the second wave. It had a better strategy to protect long-term care homes and a stronger public health system than other provinces. But cases grew there, too, in the fall as Premier John Horgan called an election and the government moved into “caretaker mode,” during which no major decisions are made. Voters gave Horgan’s NDP a majority and a second term on Oct. 24, but some criticized the election’s timing. “The question is whether B.C. deserved more than a caretaker mode from their government during a state of emergency,” said B.C. Green Leader Sonia Furstenau. In January, Horgan rejected calls to order self-isolation for travellers from out of province, which worked so well in Atlantic Canada. He also wouldn’t take action to stop visitors from travelling to Vancouver Island, although the island’s chief medical health officer asked for the measure. Cases have now spiked there.
Alberta had a miserable winter. By December, with 20,000 active cases, hospitals were filling up rapidly, and spillover field hospitals were being readied in Edmonton and Calgary. Premier Jason Kenney was forced to act, shutting down restaurants and gyms. Not everyone was happy about that. On Jan. 12, Kenney was a guest on Danielle Smith’s popular 770 CHQR Calgary talk radio show. Smith, the former leader of the Wildrose Party, peppered him with complaints about Alberta’s health restrictions: It’s not fair to rural people. Saskatchewan isn’t so strict. Allow curling like you did the NHL bubble! I can’t drop off Christmas gifts to my in-laws. “For heaven sakes, premier,” she protested, “I cut my own hair yesterday because I have no idea when you’re going to allow me to get a haircut again.”
Kenney had spent much of Alberta’s second coronavirus wave on Smith’s side of the argument, where much of his United Conservative Party base resides. He was forced to pivot to talking about the grim reality in hospitals. Six hundred COVID hospitalizations could quickly become 1,200 and 2,400, he told Smith. “We were on a fast train to a disaster in the health-care system.” But with case counts down thanks to restrictions, and the pressure on Kenney mounting, the province announced two days later that hairdressers and nail studios could reopen. After some rural restaurants defiantly opened in late January, Kenney eased dining restrictions, too. He is at a new low in public opinion polls. His management of the pandemic wasn’t effective enough to please Albertans aghast at hospitals under strain, and it was too intrusive to please the libertarians. A few of his party’s MLAs have joined a pan-Canadian group called the “end the lockdown” caucus. In late February 2021, there were rallies of unmasked anti-lockdown protesters in Edmonton and Calgary, some of them carrying tiki torches like those seen in the 2017 Charlottesville, Va., white nationalist rally.
In Ontario, Premier Doug Ford has likewise been caught between libertarians who hate lockdowns and doctors who blame him for being too slow to act. Ford ordered most of the Toronto area into lockdown in November, but it proved ineffective. While small businesses were closed, big box stores stayed open. National mobility data compiled by Environics Analytics for Maclean’s shows clearly why Ontario numbers kept going up in November: the restrictions didn’t keep people home.
Using anonymized mobility data drawn from cellphone apps of residents over the age of 15, the company measured what percentage of people are “out and about”—the term Environics uses for anyone who ventures more than 500 m from home. The overall number barely budged after a Nov. 23 lockdown: 61 per cent of people were out and about the week before; the number was only slightly lower the week after. Only when the province imposed a stay-at-home order in early January did those numbers drop, but just over 51 per cent were mobile.
Each city’s story is more complicated than topline numbers. Essential workers can’t stay at home, and the residents of wide swaths of suburbs on Toronto’s periphery—those in Scarborough, North York and Etobicoke—were more likely to be on the move. In Montreal, city-wide data from Environics shows that restrictions enacted on Sept. 23 had a moderate effect—65 per cent of residents were out and about before the new rules, and 59 per cent afterward. The real difference-maker was a province-wide curfew imposed on Jan. 9. The next week there was a 14 per drop.

Albertans enjoyed dining indoors at restaurants again as the province began to ease restrictions in early February 2021 (Jeff McIntosh/CP)
Alberta was an outlier; in Edmonton, Environics data reveals stubborn resistance to government instructions to stay at home. Last March, in the thick of the province’s first lockdown, 56.6 per cent of Edmontonians were out and about. November’s restrictions brought a barely two per cent drop from the 67.6 per cent who were on the move.
What the analysis shows clearly is that curfews and stay-at-home orders were more effective at keeping people home than loose guidelines. The provinces west of New Brunswick had been too slow in the spring of 2020, and they were too slow again in the fall.
McNeil said his province succeeded because he and Strang had established their credibility in the first wave, making the right moves at the right time. “They’re reassured that if something happens, we’ll act very quickly,” he said.
In mid-December, there was an outbreak at the same Cargill meat-processing plant near High River, Alta., where around 950 employees had tested positive for COVID in the spring. Alberta had shut the plant on April 20, hours before announcing the death of 67-year-old Hiep Bui, an immigrant from Vietnam who had spent more than 20 years working there, picking bones from hamburger. Another worker, Benito Quesada, a 51-year-old who immigrated from Mexico, died in May. His daughter, Ariana Quesada, filed a police complaint against the plant in January, alleging the company made it impossible for workers to do their jobs safely. The RCMP is investigating. But when another outbreak occurred at the same plant in December, Alberta Health Services didn’t close the plant. It didn’t make the outbreak public until February, when there were 11 cases.
Here is a comparison from the other side of the country. On Dec. 9, just a week before Cargill’s outbreak, four workers tested positive for COVID-19 at Eden Valley Poultry in Berwick, N.S. McNeil closed the plant and sent in staff to test all employees and as many people in surrounding communities as they could manage. The plant reopened 10 days later.
In November, Andrew Morris became convinced that provinces were taking the wrong approach. Morris, the medical director of the Antimicrobial Stewardship Program at Sinai Health-University Health Network in Toronto, has played a key role in figuring out the best way to treat COVID-19 in Ontario hospitals. He argued in his weekly email newsletter for a more aggressive strategy: stopping interprovincial travel and restricting travel between regions within Ontario, creating COVID-free bubbles. The premiers did not take his advice.
“It’s all based on decision-making,” he said in an interview. “You know, you can close borders or you can take control of them. A strategy like the Atlantic Bubble, it’s harder in Ontario and Quebec, and B.C. to some degree. But these were decisions, right? These were absolutely decisions that were made to not try and control the virus.”
The inaction of the premiers had terrible consequences, and nowhere were they felt more than in long-term care homes.
***

Members of the 4th Battalion, Royal 22e Régiment provided assistance to the residents of Villa Val Des Arbres in Verdun, Que., in May 2020 (Courtesy of Cpl. Genevieve Beaulieu/ DND-MDN Canada)
Chapter Three: Canada’s shame
‘All I can say is that on this earth there are pestilences and there are victims—and as far as possible one must refuse to be on the side of the pestilence’ —Albert Camus, The Plague
The worst things that happened in Canada during the pandemic happened in long-term care homes in April 2020. The facts are so bad that it is normal to shrink from them, to turn the page. The facts are that many people died not of COVID-19 but from dehydration, starvation, injuries or improper care. The people in power in whom we entrusted care of our elders did not protect them from infection and then did not competently care for them when they were infected.
All of us will die. Some of those who died in long-term care homes would have died before long. Their deaths were tragic not simply because they died, but because they died neglected, alone and suffering. Their loved ones were prevented by law from being at their sides to offer support or ease their path.
They died in circumstances that would cause public outrage if they were revealed in a livestock operation. It would be wrong to say they died in conditions like those in the developing world, because many people in the developing world do a better job of looking after their elders.

Juanita and Howard Robinson use a phone to speak with family gathered outside the window at their LTC home, on April 3, 2020. Juanita and Howard died within five hours of each other, on April 6, 2020, in North Vancouver. (Courtesy of Sharon Robinson)
Many in the developed world do, too. A report published in September by the U.S. National Institutes of Health found that the death toll in Canada’s long-term care (LTC) homes was by far the highest among 12 OECD countries studied; LTC home residents made up 78 per cent of our national COVID deaths, compared to the 12-country average of 47 per cent.
This is Canada’s shame.
The first Canadian to die of COVID-19. on March 8, 2020, was a man in his 80s living in a Vancouver care centre. By February 2021, when most LTC residents across the country were vaccinated, more than 14,000 had died. If it were not for our failure to protect long-term care residents, about 7,700 deaths would have occurred in this country.

Ambulance attendants wheel a patient out of Floralies LaSalle seniors’ residence in Montreal amid a coronavirus outbreak at the facility (Christinne Muschi)
Many of the deaths happened in Quebec and Ontario. Early in the pandemic, while other countries, and some Canadian provinces, were taking steps to protect LTC residents, their governments did not act effectively, even after the first grim signs of an unfolding crisis emerged. At Pinecrest Nursing Home in Bobcaygeon, Ont., in the cottage country north of Peterborough, Ont., residents started dying in March. The virus got in, perhaps brought in by a visitor or a staffer with what appeared to be an innocent sniffle. By the end, 28 of 65 residents of Pinecrest were lost to COVID.
On April 11, a report from Dorval, on the West Island of Montreal, made it clear how bad things would get. The Montreal Gazette’s Aaron Derfel learned that residents’ family members had observed a stream of funeral vans coming and going from Résidence Herron, a private home that was so badly off it had been abandoned by frightened workers. When inspectors arrived, they found few people working, and patients in filthy diapers, so dehydrated they couldn’t speak. Families, who were spending as much as $10,000 a month to keep their loved ones there, were horrified. Quebec’s coroner found 38 residents died at the home between March 26 and April 16. The outbreaks in Bobcaygeon and Dorval made it clear that many people would die in misery and squalor if things carried on the same way.
On March 30, Ontario Premier Doug Ford tweeted: “We’re putting an iron ring of protection around our seniors.” There had been 17 deaths in Ontario care homes at that point.
***
On April 15, with 14,860 COVID cases and 487 deaths in his province, Quebec Premier François Legault asked Prime Minister Trudeau to send military help for LTC homes. Trudeau said he was considering the request. I couldn’t understand the delay. Media reports were clear: the homes needed help.
The next day I called Annie Bouchard, a retired Canadian Armed Forces (CAF) colonel. I had met Bouchard in 2010 in Jacmel, Haiti, when she was serving with the CAF’s Disaster Assistance Response Team, treating Haitians after a devastating earthquake. I had been impressed by her warm-hearted but no-nonsense approach to the tragedy, her sang-froid in the midst of heartbreaking disaster. I reached her in Luxembourg, where she is now a civilian medical adviser to NATO.
“If the premiers of Quebec, Ontario and the Prime Minister of Canada decide this is the way to go, they could solve this in a heartbeat,” she told me over the phone. “It’s just that . . . they need to agree this is the way to go.” She was sure the military had the capability to handle it. “When we deployed to Sierra Leone, during the Ebola crisis in 2014, not one of us got infected,” she said. “Not one of those folks got infected with the virus. So, yes, we can use PPE in a very efficient way. We are soldiers. We can do anything.”
The difficulty, in her experience, is politicians who don’t want to ask for help. “They will have to admit they are overwhelmed. They don’t like to do that.”
At the time, Dr. Samir Sinha, director of health policy research of the National Institute on Ageing and director of geriatrics at the Sinai Health-University Health Network in Toronto, was talking to officials in Ontario, urging them to act. “I have the privilege of caring for a number of Holocaust survivors,” he told me in a recent interview. “Basically, it taught me . . . never stay silent when you feel lives are at risk.” Sinha believes politicians delayed calling in the Forces for political reasons. “They were ready to be deployed a month before Ontario applied formally,” he said.
Lt.-Cmdr. Heather Galbraith, a family physician at Canadian Forces Health Services Group in Ottawa, was baking a birthday cake for her daughter when she got the call telling her to pack her bag. She and Maj. Karoline Martin were soon off doing “recces”—site visits to hard-hit homes in Ontario and Quebec.
The homes they visited were among the worst. It was tough for the military personnel, Maj. Martin said later in a presentation to a commission looking into the Ontario LTC disaster, chaired by Justice Frank N. Marrocco. “Those clinicians, when they went into these facilities in crisis, were taken aback,” she told the commission. “They were taken aback because there was a significant deviation from the way they were used to practising medicine.”
CAF personnel recorded their observations in a report of what they saw at five LTC homes in Ontario that was made public in May. It paints a picture of neglect and maltreatment that is emotionally difficult to absorb. The homes had been understaffed for weeks. Skeleton staff, supported by temporary agency staff, could not maintain whatever standards of care had existed before the pandemic. Supplies were kept locked up by cost-conscious management. CAF personnel observed residents who were dehydrated, malnourished, dirty, suffering from untreated injuries. They saw cockroaches and flies, and stacks of stinking, dirty old meal trays left next to patients’ beds. Infected and uninfected patients were together. Disabled residents had not been turned, or put in their wheelchairs. Staff were not using PPE appropriately or disinfecting medical devices to prevent infection.
The businesslike medical language of the report is stark:
“Mouth care and hydration schedule not adhered to.”
“Wound care supplies insufficient or locked away.”
“Feed bottle not being changed for so long the contents of the bottle had become foul and coagulated.”
“Staff reported that medications are being reported/documented as being given but they are not.”
“Staff report residents having not been bathed for several weeks.”
“Significant gross fecal contamination was noted in numerous patient rooms.”
“Expired medication.”
“Observation of incident that appeared to have contributed to patient death (code blue due to choking during feeding while supine—staff unable to dislodge food or revive resident).”
For the families who had loved ones in the care homes, the report gave terrible answers to questions they had been asking since March, when the province ordered the homes closed to visitors.
***
When Pamela Bendell read the report, she told Maclean’s, she understood what happened to her mother. June Bendell had died at the age of 91 a few weeks earlier, on May 8, in Orchard Villa Long Term Care Home, a privately owned home in Pickering, Ont., just north of Highway 401.
Pamela got a call on May 6 from a nurse, who said her mother wasn’t doing well.
“I said, what do you mean? And she said, ‘Well, she’s not breathing properly.’ ”
On May 8, she got a call from another nurse. “I think your mom’s passing away,” the nurse told her.
“I said, ‘Can I not come over? I’m a couple streets away.’ They said, ‘No, you can’t.’ She . . . died literally while I was on the phone.”
Bendell, who is part of a class action suit against the home, believes the CAF report explains how her mother died. June Bendell suffered from Lewy body dementia and had become rigid, which meant she had to be fed with care to avoid choking. One line in the document stood out to her: “Observation of incident that appeared to have contributed to patient death . . . code blue due to choking during feeding while supine.” She thinks that patient was her mother. That allegation has not been proven in court. Both Southbridge Care Homes, the owner, and Extendicare, the company it hired to run the home, declined to be interviewed. In a joint emailed statement, they said that in keeping with privacy legislation, they “cannot discuss or disclose information regarding the health of a resident to anyone other than the resident or their power of attorney.”

June Bendell at Orchard Villa Long Term Care Home (Courtesy of the Bendell family)
Pamela previously worked in a nursing home. She was better able than most families to try to make sure her mother was cared for, seeking allies among staff and other residents. She is angry her efforts were in vain, that her mother died as she did. June was a loving mother of two. She enjoyed knitting, camping and travelling. She and her husband used to dress up as Santa and Mrs. Claus and visit nursing homes at Christmastime to cheer up the residents. “It’s a blessing she’s not being tortured anymore,” Pamela said. “But what a hell of a way to go for anybody on this earth . . . in sh–ty diapers and bugs and everything else.”
Orchard Villa is far from the only home facing intense scrutiny, and legal action. There have been dozens of suits, as well as a proposed class action, involving almost 100 Ontario institutions. But it was, in those first few weeks of the pandemic, among the hardest-hit. According to Durham Region data, there were 71 deaths and another 135 infections among residents at Orchard Villa’s LTC home in spring 2020, with another seven deaths and 22 infections at the Orchard Villa retirement home next door. The families believe many of the deaths could have been prevented. In many cases, there continues to be confusion about how residents died, and families don’t trust the accounts from the home.

Christine Tappin and her mother took her father out of Orchard Villa for the evening to celebrate what would be his last birthday, on October 8, 2019. (Courtesy of Christine Tappin)
On Father’s Day last year, Christine Tappin dropped off a care package, complete with her dad Samuel’s favourite candies, at the front door. Then she made her way to his window and watched him open it, realizing she’d forgotten the card at home. They talked on the phone, through panes of glass. They kept chatting as she rose to leave, got into the car and drove home. “Dad, I’m home now,” she said, after parking in her garage. “Let me hear you get through the door,” he said. She did. It was the last time they spoke.
Christine’s mother, Helen, had visited her husband every day until the home was locked down last April. She called him on the phone every day thereafter. But on their 41st wedding anniversary—two days after Father’s Day—she couldn’t get through. She tried six times. No one would take Samuel the phone. “Not right now,” care workers told her. “Take the phone away.” Helen never got through to Samuel. He died that day.
Like dozens of others at Orchard Villa, Samuel had been diagnosed with COVID-19 back in April. But his family still doesn’t know the cause of his death—whether, by June, he was still suffering complications of the disease, or whether something else went wrong. Eight months after Samuel’s death, they are still in the dark. “I have no closure,” Helen said. “I feel like he’s protected me his whole life,” said Christine. “And then at the end, I couldn’t protect him.”
The ten families and whistle-blowers who spoke to Maclean’s describe deteriorating conditions at Orchard Villa since 2015, when the family-run company that owned the home sold it to Southbridge, a private equity firm that lists 36 Ontario homes in it portfolio. To handle Orchard Villa’s operations, Southbridge brought in Extendicare, which manages 96 homes in Manitoba, Saskatchewan, Alberta and Ontario, including the Tendercare home in Toronto, the site of a deadly COVID outbreak this winter.
Extendicare’s first home was in Ottawa, but it expanded into the U.S. in the 1970s. In 2015, it sold its American portfolio of homes for US$870 million. It left the United States after paying US$38 million in fines to the U.S. Department of Justice and eight states for false claims. The New York Times reported at the time, “Care was so inadequate, officials said, that some patients became malnourished and dehydrated and developed infections that led to unnecessary hospitalizations.”
Bendell said the food and the quality of care at Orchard Villa “started to go downhill” after 2015. Troy Wannan, who started at Orchard Villa as a nurse in 2001 and worked her way up to managing the retirement residence next door, observed changes, too. She said creature comforts and routine sanitary procedures were cut after the home changed hands. Monthly bus trips for residents were cancelled, as were the annual spring cleanings and laundering of curtains. Carpets were no longer professionally shampooed. Private rooms were no longer deep-cleaned in between residents. “There’s carpeting that had been in the building for years. So if we had incontinent residents, it should be professionally cleaned,” Wannan said. “But I was not allowed to do that.” The emailed statement from Southbridge and Extendicare said there was “a robust recreational and activity calendar for residents” before the pandemic, and that they have “always maintained spending on cleaning and housekeeping services.”
Wannan said there was pressure on her to keep beds full, which ultimately meant bringing in residents who required more care than the staff could provide. But she said the company simultaneously reduced the number of personal support workers who could be on shift at any given time. “It was all money, money, money,” Wannan said. She had loved her job. “I loved the families, the residents,” she said. But the ever-increasing workload and the worsening environment led her to resign in September 2019.
Another nurse at Orchard Villa who spoke on condition of anonymity observed that after the home was sold, adult diapers, gloves and masks were kept under lock and key. In the morning, residents would often wait to have their undergarments changed while workers asked supervisors for supplies, who in turn asked the maintenance team to unlock supply areas. “They count everything you use,” said the nurse. Some staff would buy their own equipment.
When the pandemic hit, before there were any confirmed cases at Orchard Villa, staff were told not to use up the small supply of PPE, the nurse said. In one case, the nurse recalled a manager saying, “Why are you wearing masks? You’re scaring the residents.”
In their statement, Southbridge and Extendicare noted that supply logs show they “always maintained a good supply of PPE,” and that staff were trained in its proper use and “received ongoing education throughout the pandemic.”
***
One day in early April 2020, a nurse at Orchard Villa was attending to a patient with a fever. After work, the nurse received a call from a family member, who said that patient was now in hospital with COVID-19. Only later did the nurse hear from Orchard Villa about the possible exposure. The nurse tested positive. So did one of the nurse’s family members, who was later hospitalized. The outbreak had begun.
At the beginning of April, Cathy Legere, a retired infection control nurse who’d worked at a children’s hospital, arrived at Orchard Villa to volunteer her services. She knew the place because her father-in-law was a current resident on the long-term care side; her mother-in-law had stayed there, too.
She arrived to find roiling anxiety and anger among frontline staff, whose preventative measures in early April, she said, consisted of “heightened awareness of hand-washing” alone. “Can you imagine being told to go and fight your enemy on the frontlines with no guns?” Legere said. “Everybody knew there were masks and gloves locked up in a supply room, but they weren’t to be used because they’d run out.”
She told staff to find cheap sunglasses to wear as makeshift goggles. And she gathered volunteers to sew cloth masks. They started sewing gowns, too, but management rejected that idea without saying why. She tried to educate the staff on infection control but she feared it was already too late. “I just knew that the chance of this being a super-spreader event was huge. The lack of PPE, lack of education and lack of policy. It’s unexplainable, unacceptable.”
Another issue raised by staff and residents was an increasing reliance on temporary agency workers, many of whom worked in several other homes, which is believed to have helped spread the virus from home to home. In April, Ontario issued an order to prevent health-care workers from working at more than one home, but there was an exception for temp agencies. Dr. Nathan Stall, a geriatrics expert at Sinai Health, studied anonymized cellphone data that suggested workers from temporary agencies continued to work in multiple homes, which opened paths for contagion.
After the first COVID case in the home, Legere said, she pleaded with staff to move and isolate the patient, who was sharing a room with three others. It didn’t happen. Soon, the others were infected. Residents still ate meals communally, although social distancing measures were in place. During her second week, Legere said they started delivering meals to the rooms instead. Legere didn’t volunteer for a third week. She caught COVID-19 herself. While recovering at home, she was appalled to hear of the conditions endured by her father-in-law, Nick, who survived an asymptomatic case of COVID-19. He had been moved out of his private room into a shared room. When his roommate contracted a severe case of the disease, the man wasn’t moved out. For two days, Nick watched him struggle to breathe. And when the man stopped breathing, Nick was in the room with the body for “a long, long time,” Legere said.
“Orchard Villa implemented all protocols regarding the passing of a resident at a long-term care home,” the statement from Southbridge and Extendicare said. Since September, it noted that Southbridge has directly overseen frontline care and services at Orchard Villa. It has hired two epidemiologists to support staff at homes, has staff tested three times a week and, with support from Extendicare, has in place “strong policies to fortify the quality of care residents and families receive.”

Residents of Orchard Villa Long Term Care Home who died in the COVID-19 outbreak are remembered at a vigil on June 15, 2020 (Frank Gunn/CP)
For too many of the 160,000 people in LTC homes across Canada, the pandemic brought a dramatic decline in a quality of life that was already compromised. Given that 70 per cent of long-term care residents have dementia, workers struggled to keep the infected from mixing with others. In some homes, overworked staff took away wheelchairs and canes to keep residents put. In one assisted-living home near Oshawa, Ont., staff removed door handles to keep residents in their rooms. The effects of the prolonged isolation had “really extreme collateral damages” leading to rapid physical and mental decline, Stall told the Marrocco commission. “I have spoken to caregivers who, when they were finally allowed back in, their loved one no longer recognized them.”
One resident who survived a COVID infection described a long, grim year in Orchard Villa under lockdown, trapped in a private room: “I haven’t murdered anyone, but I’m in prison.”
The pandemic hasn’t been much easier for workers, many of them precariously employed racialized people who risk infection for as little as $14 an hour, dramatically less than the wages earned by equivalent workers in hospitals. More than 24,500 staff at Canadian care homes contracted COVID. A source who would only speak under anonymity for fear of retribution said that, even before the pandemic, the staff at Orchard Villa were dedicated, but stretched too thin. “I’ve never seen people work so hard. When I compare it to a hospital, when you look at the pay, when you look at the workload, when you look at the responsibility, I felt like it was vulnerable people looking after vulnerable people.”
***
Last spring and summer, as COVID-19 ravaged long-term care homes across the province, several of Ontario’s major operators of LTCs took action. They hired lobbyists. Most had connections to the Ford government. Stella Ambler, a former federal MP currently seeking a nomination with the Ontario PCs, registered as a lobbyist for Southbridge, which owns Orchard Villa and other homes. Leslie Noble, one of the most powerful lobbyists in the country, was hired to represent Chartwell Retirement Residences. Earlier in her career, Noble ran two campaigns for former premier Mike Harris, who is the chair of Chartwell’s board. Andrew Brander, former director of communications for former finance minister Rod Phillips, registered to lobby for the Ontario Long Term Care Association, and Melissa Lantsman, a former Ford campaign spokeswoman who is seeking a federal Conservative nomination, registered to lobby for Extendicare.
The lobbying effort tightened an already close relationship between Ontario PCs and the industry. Former PC premiers Ernie Eves and Bill Davis have both served on LTC company boards. Michael Wilson, who was the Ontario attorney general’s chief of staff until January 2020, is a more recent entrant. Wilson, who was subject to a one-year cooling-off period under the law that prevented him from lobbying his former boss, registered for two care home companies in May: Revera and Sienna Senior Living. He registered to influence “any future legislative changes impacting long-term care.” He declined to be interviewed for this story but told me in an email he did not lobby his former boss.
People are not the only resource connecting government and industry. A Huffington Post analysis found LTC industry lobbyists had donated more than $30,000 to the Ontario PCs. And in the first three quarters of 2020, the Toronto Star reported, Extendicare, Sienna and Chartwell received $138.5 million through provincial and federal pandemic funding. Over the same period, those three companies paid out nearly $171 million to shareholders.
***
When the Canadian Armed Forces report leaked, Premier Doug Ford looked rattled. “It’s so disturbing when I read this, it was hard to get through this,” he told reporters. “It was the worst report, the most heart-wrenching report I have ever read in my entire life.” He promised action. “There’s going to be justice. There’s going to be accountability.”
Gary Will, the lawyer for the families who have filed a $160-million lawsuit against Orchard Villa, Extendicare and Southbridge, was relieved by that response. According to Will, Orchard Villa had been investigated 19 times between 2017 and 2019 by Ontario’s ministry of long-term care, so under Ford, as well as premier Kathleen Wynne. The statement of claim notes that the ministry spent 43 days investigating complaints and issued 28 written warnings, 17 voluntary plans of correction and eight compliance orders. But there were no fines or charges.
Will was heartened by Ford’s pledge. “He sounded very sincere that he was going to get to the bottom of it,” he said in a recent interview. “The police were going to investigate. Charges would be laid if appropriate. I thought, okay, this is a guy that is actually going to do something.”
One thing Ford did, in October, was table Bill 218, the “Supporting Ontario’s Recovery” act, which made it harder to sue individuals or businesses, including long-term care homes, with COVID-related claims. The act set a new standard for liability—gross negligence, which is as yet ill-defined—as opposed to good old-fashioned negligence. Many observers say the act would make it difficult for courts to find against homes if they made “an honest effort, whether or not that effort is reasonable,” to protect residents.

Ford’s Ontario PC party has come under scrutiny for its ties to long-term care industry lobbyists (Nathan Denette/CP)
In June, when CBC first reported that the government was planning to move to protect the operators, Will didn’t believe the story. He didn’t think Ford would block lawsuits. “I said to myself, I don’t think he’s going to do that because I think he’s quite sincere about what he said.” The government passed the bill, over the objections of families and seniors’ advocates, which ought to make life easier for the lawyers preparing to defend the care homes in court. “I would bet the lobbyists basically wrote that law,” said Will.
The industry says the law was necessary, because many homes were facing the prospect of losing liability insurance, without which they can’t operate. “Liability protection is a necessary measure to stabilize and renew Ontario’s entire long-term care sector,” Donna Duncan, CEO of the Ontario Long Term Care Association, told Maclean’s in an emailed statement. “Without it, many insurance companies will cease coverage, as they have already begun to do, putting homes across the province at risk and jeopardizing their expansion and renewal.”
The bill was necessary, said Nicko Vavassis, a spokesman for Ontario Attorney General Doug Downey, via email. “We heard from stakeholders across various sectors that this protection was necessary for them to continue their operations,” he wrote. “That said, our government believes in holding bad actors accountable.”
The province says it moved quickly to protect residents in the homes when the outbreak started, spending millions on staffing and issuing directives to tighten infection control. Critics say the measures were too little to protect residents, and testimony at the Marrocco commission suggests provincial officials failed to properly allocate and coordinate resources for testing and PPE, leading to deaths in the homes.
More than 4,000 long-term care residents have died in Ontario since Ford promised to put an iron ring around the homes. In Will’s view, Ford failed to protect the residents; the new legislation puts an iron ring around the owners of homes instead.
***
On April 14, with care breaking down in Quebec’s homes, and 435 total deaths in the province, Legault pleaded with Quebecers to volunteer to work in the homes. “I appeal to your sense of duty to help us protect our most vulnerable,” he said.
Ryan Hicks, a law student at McGill University, answered the call. “I had two grandparents who lived in long-term care near the end of their lives,” he told me in an interview. “I was personally aware of how important it is that our elders are cared for appropriately.” So he sent an email to the West Island health authority on April 19. “My name is Ryan Hicks—I am 37 years old, healthy and would like to volunteer.” They signed him up and, after an afternoon of training, he was sent to Grace Dart Extended Care Centre in Montreal’s East End, where dozens of residents had been infected.
I met Hicks a decade ago in Ottawa, when he was a producer on CBC’s Power & Politics show. A friendly, thoughtful guy with a self-deprecating sense of humour, he was popular on Parliament Hill. He later worked as a CBC reporter, in Charlottetown and then at the National Assembly in Quebec City. He soon starts a summer job at a New York City law firm.
The week before he got to Grace Dart, staff held a short memorial service to remember 64-year-old Victoria Salvan, who died of COVID after 25 years of work at the home, one of about 27 LTC workers who died during the pandemic. When Hicks arrived, a stressed-out coordinator sent him to change into his scrubs in a converted lunchroom. Then he went upstairs into the red zone—marked by red tape—where many patients were infected.
It was not an easy day. His first patient, a woman with advanced dementia, was screaming. “She’s grabbing the bed. You can tell she’s scared,” he recalled. “We’re trying to change her because who knows how long she hadn’t been changed for? And I had never done that. I don’t have experience with that.” Hicks did what was necessary, helping the personal support worker (PSW). The next day he was so exhausted—psychologically and physically—he paused outside before going in. He wasn’t sure he could face another day. It was difficult work. “After the fifth diaper change, the PSW, who was fantastic, said to me, okay, so can you do this on your own? And I was like, I think it’s going to take me a little bit more time.”
Canadian Armed Forces personnel were dispatched to Grace Dart, and Master Cpl. Samuel Boulet, 27, a reservist from Quebec and a medical assistant, arrived there on April 27. As at Orchard Villa and other Ontario long-term care homes where the CAF helped, military personnel ended up working closely with permanent staff and the situation got better. Boulet said you could see the improvement in the patients. “I could see people getting better. They walk more. They talk more. There were patients in the hall. That’s a good way to see that elderly patients are doing well. They eat. They move. They talk.” By the end, Boulet said, he would have left his grandfather in the hands of the people he worked with.
***
Lockdown opponents often say we should protect seniors in care while letting the virus spread in the community. That may not be possible. “We know that the strongest risk factor for whether a home is going to experience an outbreak is the transmission of COVID-19 in the communities surrounding [care] homes,” said Nathan Stall, the geriatrics expert at Sinai Health. “These are not impenetrable environments despite the most world-class [infection prevention] measures. Suppressing community transmission of COVID-19 is really essential if you’re going to prevent outbreaks.”
If both operators and governments were unprepared for the first wave, they shouldn’t have been for the second. Stall had called for Ontario to repurpose empty hotels, to get residents out of the four-to-a-room facilities where hanging blankets separated beds. Ontario took some steps, but didn’t do the things that would have stopped a second wave. “The provincial government spent the summer doing a PR tour,” said Natalie Mehra, executive director of the Ontario Health Coalition. At least Quebec trained more staff, she said. “It still has not happened in Ontario . . . we need more than 20,000 staff.”
Ontario lost more than 2,000 LTC residents in the second wave, after 2,072 deaths in the first, the National Institute on Ageing reported. In comparison, Quebec lost 3,103, down from 4,613. Ford has announced the government will build facilities for 30,000—eventually. Some of those beds—87 new units—will be at Orchard Villa, to the shock of families involved in the class action.

A memorial of crosses outside a care home affected by COVID-19 in Mississauga, Ont., in May 2020 (Ian Willms/Panos Pictures)
LTCs in the Western provinces were also hit hard in the fall and winter. Saskatchewan had only two resident deaths in the first wave, but 84 in the second. Manitoba had three, then 468. Alberta went from 153 deaths to 1,013. The province now leads Canada with the highest percentage of its homes experiencing outbreaks, the National Institute on Ageing’s Sinha noted; “They were [all] frankly asleep at the wheel.”
The crisis in long-term care homes was a long time coming. The problem is in part one of money. British Columbia, which performed the best during the pandemic, spends more per resident—$222 per day in 2018-2019 compared to $203 in Ontario, according to the Canadian Medical Association Journal (CMAJ). British Columbia did a better job of keeping COVID out of the homes, tested aggressively and isolated anyone who might have been infected.
Many people who know the system at the grassroots level believe penny-pinching by private operators results in inferior care, and experts see a difference. “Evidence suggests that, on average, for-profit homes deliver inferior care across a variety of process and outcome measures,” the CMAJ concluded. “The evidence [even] before COVID-19 very clearly shows they have worse outcomes across a wide variety of clinical and process outcomes,” said Stall, “whether it’s mortality or transfers to hospital, lower levels of quality of staffing, or complaints.”
But the horrors were not confined to for-profit homes—the disaster in Quebec happened largely in public homes. And some privately operated homes effectively protected their residents.
Everyone knows what is necessary: more beds; one bed per room, to cut down on seasonal viruses; better inspection regimes, with penalties for operators who provide substandard care; better home-care programs, to reduce the number of people in facilities; improved pay and conditions for workers, so they don’t have to hustle to work at multiple homes.
There just hasn’t been the will to do it. “It’s exposed an incredible, vicious ableism in our society,” said Nora Loreto, a Quebec City activist and journalist who, since the spring, has been compiling a database of deaths in long-term care homes across the country, spending hours every night doing volunteer data entry. “People in assisted living are not a priority. They’re not a political priority. They’re not a social priority. They absolutely are not an economic priority. The reaction to those deaths is sadness, and that’s it.”
Jurisdictional struggles get in the way of solutions. The federal NDP has called for national standards, a federal backstop, to accompany an infusion of new money. The federal Conservatives say the feds should stay out of it. Trudeau’s Liberals have called on the provinces to establish minimum standards, but they haven’t said what they will do if that doesn’t happen.
Political solutions depend on pressure, which is not likely to come from the residents. Unlike health care, long-term care is rarely an important election issue. That makes it, as Stall told the Marrocco commission, an easy sector to neglect. “The majority of people who live in long-term care, with 70 per cent having dementia and 90 per cent having cognitive impairment,” he testified, “are not necessarily able to advocate for themselves. Most of them may not vote, and a lot of them may not be alive for the next election.”
***

Karilynn Simpson waits in the schoolyard with her son William on his first day of Grade 4 in Calgary, on Sept. 2, 2020 (Leah Hennel)
Chapter Four: How will Canada fare next time?
‘The health of the people should be the supreme law’ —Cicero
On April 17, just five days after British Prime Minister Boris Johnson was released from hospital, where he had been treated for COVID-19, the U.K. government made an announcement: it had established a vaccine task force, whose members included Sir John Bell, a Canadian immunologist and professor at Oxford University. It had been a challenging spring for Johnson, who had made a point of shaking hands against public health advice, and wagered on a herd-immunity approach that would allow the virus to move through the community without overwhelming the health-care system. Midway through April, after a report from Imperial College London predicted disaster if things continued as they were, the government changed gears.
Dr. Alan Bernstein watched the announcement with interest. A month earlier, the U.S.’s Food and Drug Administration had approved clinical trials for Moderna. “I read about the vaccine task force in the U.K. and I know people who were on that,” he said later in an interview. “So I talked to them and that’s when I decided to write [to the Canadian government].”
Bernstein is the president and CEO of CIFAR, a Canadian research granting organization. Before that, he headed an HIV vaccine organization in New York, and the Canadian Institutes of Health Research, a federal agency. He knows a lot about vaccines, and a lot about how government works. He sent an email to Canadian officials suggesting that Canada follow the U.K. lead. “The government acted very quickly,” he said. “There was a mandate put together. I think there’s roughly 12 of us and co-chairs were put together and it went through cabinet . . . It took them about three or four weeks to do all that, which for the government is pretty fast. And we started, and it ruined my summer, basically.”
Bernstein and the other task force members—pharma executives and scientists—met online twice a week, going through submissions from would-be vaccine manufacturers—hundreds of pages of documents—looking for winners. There have been complaints from unsuccessful Canadian applicants, but the task force members say they were prioritizing companies that had the capacity to produce. They found them. The task force made recommendations to the government, which negotiated the deals. That led to contracts with eight companies, including five that by February 2021 would either be distributing vaccines or awaiting Health Canada approval: Moderna, Pfizer-BioNTech, AstraZeneca, Johnson & Johnson and Novavax.
Canada ensured access to huge numbers of vaccines—eventually. In February, Canada was trailing not just Israel, the United States and Britain, but France, Germany, Morocco, Turkey, Serbia and Chile. Canadians could see, every day, evidence of rapid progress in the United States. For most of the pandemic, Canadians watched the U.S. bungle pandemic management: the United States had three times Canada’s death rate, and a number of Americans poisoned themselves with bleach after one particularly inane comment by their president. But, as if by magic, when Trump left, the U.S.’s pandemic response improved dramatically. Within a few weeks, the New York Times was asking if the Biden administration was being ambitious enough in administering 1.7 million vaccines per day; it quoted experts who thought three million a day was a feasible goal. As of Feb. 19, Canada had distributed 1.8 million vaccine doses. The United States government had distributed 78 million.

People wait in line in Olympic Stadium in Montreal for vaccines on March 1, 2021 (Christinne Muschi/Reuters)
The opposition attacks wrote themselves. For everything Trump did wrong—and at times he appeared to be an agent for the virus—he got one big thing right. He launched a vaccine moonshot—Operation Warp Speed. Could Canada have done better?
Bernstein says voters should understand Canada doesn’t have that much leverage with the pharma giants. “The U.S. has 10 times the population,” he said. “So they have 10 times the buying power we do. So where we’re buying a total from any one company of 40 million vaccines . . . Let’s say then the U.S. is buying 400 million. If you’re the company, who are you going to pay more attention to? I think the answer’s obvious.”
When cranky Canadians were asking Trudeau to explain the delays, the pharmaceutical industry had an answer: federal drug policy. A few days after Christmas, the industry complained. “New drugs are not being launched in Canada, clinical trials have declined and investments in our vital life sciences sector are being scaled back,” warned an industry lobby group called Innovative Medicines Canada. In January, just before Pfizer announced delays in planned vaccine deliveries, the Financial Post ran a scathing op-ed by Paul Lucas, the retired head of GlaxoSmithKline. He blamed generations of Liberal governments for “hollowing out” pharmaceutical innovation in Canada by eroding patent protection and favouring generic producers who sell cheaper drugs.
Sharon Batt, a writer and researcher in Halifax who focuses on the role of patients’ advocacy organizations in pharmaceutical policy, pointed out that big companies oppose reduced prices. “They obviously don’t want to lose money. The whole idea is to pay less for drugs,” Batt said. “Why would the industry want that? They’re fighting tooth and nail.”
Big pharma doesn’t like the new pricing measures proposed by the Liberals for the Patented Medicine Prices Review Board, a federal agency established in 1987 to keep drug costs down. They are likely also unhappy with the 2019 Liberal election promise to “take the critical next steps to implement national universal pharmacare,” which can be expected to be bad for drug companies (if the Liberals actually do it—most Liberal MPs voted against an NDP motion calling for pharmacare in February).

Karl Kuhnlein, 90, wears a party hat to receive his vaccination on Feb. 25 in Calgary; he’s looking forward to playing pool with friends (Leah Hennel/Alberta Health Services)
As Pfizer cut January vaccine deliveries, it called for Ottawa to cut corporate taxes, and criticized the CRA for being too aggressive in policing transfer pricing, a technique multinationals use to shift profits to low-tax jurisdictions. Could Canada have avoided those delays if the industry wasn’t busy fighting Ottawa?
Senior federal officials and vaccine producers insist the tension on drug prices is distinct from Canada’s procurement of the hottest commodities on earth. Anita Anand, the procurement minister, told Maclean’s that every conversation she’s had with every pharmaceutical company—including countless text messages—is about vaccines. But Anand has admitted that Novavax was the only one of six foreign vaccine providers open to licensing its product for domestic production, at the National Research Council’s Human Health Therapeutics Research Centre, in Montreal.
The government of Canada owns a 500-litre bioreactor in that facility that critics say Ottawa could now be producing vaccines if the government hadn’t made a bad bet on China. They make a persuasive case.
In August, University of Ottawa law professor Amir Attaran, who has a Ph.D. in immunology, wrote to senior health officials urging them to contact Sir John Bell, a key player on the team behind the AstraZeneca vaccine whom he remembered from his Oxford days. Attaran wanted the feds to persuade Bell to let us manufacture the vaccine at the Montreal facility. The NRC website says the facility is “extensively used by biotechnology companies for pilot-scale production and purification of recombinant proteins, viral vectors and vaccines.”
But in May, Ottawa announced it was planning to use that bioreactor to make vaccines for CanSino Biologics Inc., a Chinese company that had previously collaborated with the NRC on an Ebola vaccine. Dalhousie University in Halifax was to run the trials—which would have turned out to be tough in COVID-free Nova Scotia—but that didn’t end up mattering, because Chinese customs blocked a shipment a few days after the deal was signed, something the feds only told Canadians in August. By then, the advisory committee had already recommended against that vaccine.
The opposition thinks Canada was foolish to trust China. “We first put all our eggs in one basket with the CanSino deal,” wrote Conservative health critic Michelle Rempel Garner in January. Attaran thinks they tied up the only federal machine they could have used to produce vaccines. (The NRC says the bioreactor doesn’t have the right certification to make vaccines for humans, but NDP MP Don Davies, who has sat through many health committee meetings, pointed out that Trudeau announced it was going to do just that in August. “What vaccine was he talking about and what capacity was he referring to?” he asked. “It must have been that project with CanSino.”)
The government is renovating the Montreal facility, and has reached a deal to produce vaccines there for Novavax, although not until later this year. “I’m not going to get into a discussion about whether you guys did the right thing or the wrong thing,” Bell told CTV’s Evan Solomon in January. “The reality is you don’t have enough vaccine. You know you need to get on with it.”
Whatever the government needed to do to get vaccines on time, it didn’t do.
***
The two big countries that have done the best on pharmaceutical solutions—the United Kingdom and the United States—failed in every other way to deal with the pandemic, and lost many more people. They bungled the non-pharmaceutical interventions—like masking and social distancing—and succeeded with pharma. Governments can’t necessarily walk and chew gum and roll out national income-support programs and manufacture vaccines all at the same time.
Canada handled the beginning and the middle of the pandemic better than the U.K. or the U.S., but those countries are having a good ending. They will likely emerge from the pandemic months before we do. Their citizens will likely be taking in concerts and football, visiting relatives, singing in church and knocking back pints at the pub while we are still huddled in our homes, gaining weight, going deeper into debt and worried about variants that might cause a terrible third wave. Canada finishes the pandemic as we started it—behind the play. We have never been where the puck was going.
Dominic Cardy, who was right when a lot of people were wrong, said recently that Canadian politicians have been afraid to lead. “You’re elected to do things that are difficult,” he said. “And the failure of a lot of governments to do anything vaguely difficult in the beginning left them in a position where they were left with horrible choices from the summer onwards. And the part I found kind of shocking was a total failure to learn from experience.”
It has been a failure that has cost us dearly. By the time the pandemic is over, it will likely have cost about 25,000 Canadian lives. We faced the biggest national challenge since the Second World War, when we lost 44,000 lives, and we didn’t do as well as we could have.
We did better than a lot of countries—better than Germany, worse than Denmark—but we have so many advantages that it feels like a failure. We could have been like Australia, which lost fewer than 1,000, or South Korea, which lost 1,600, or Taiwan, which lost nine.
A lot of the countries that did well are used to worrying about threats to their national security—particularly threats from China to their national security. The people in those countries are psychologically quicker to recognize a threat because they are used to fretting about them.
Canada, for its part, is among the most blessedly peaceful countries on the planet. We have few, if any, enemies. We are rich and comfortable, and not used to having the government make us do things. That makes us slow to notice a threat on the horizon, and bad at organizing a response. It struck me that some of the people I spoke to for this article who were quickest to see how COVID could damage Canada—like Dominic Cardy, Julie Smith and Jane Philpott—have worked in developing countries, where people can’t take it for granted that everything will always be okay.
The capacity to recognize a threat and respond through collective action—more than resources—seems to have been the key. In 2019, the Johns Hopkins Center for Health Security teamed up with the Nuclear Threat Initiative and the Economist Intelligence Unit to create the first Global Health Security Index, to rank 195 countries for their theoretical ability to deal with the “emergence and spread of pathogens.” Of the top 10 countries on that list—which included the United States, the United Kingdom and Canada—only Thailand and Australia actually stopped COVID. The U.K. and the U.S. are on the top 10 list nobody wants to be on: countries with the highest rates of deaths per million (1,860 for the U.K., 1,580 for the United States). Canada did better, at 595; we had fewer than Greece, more than Costa Rica.
One of the strange things about this disease is how some poor countries stopped the disease in its tracks because they were well-organized. Tiny Bhutan, which has a GDP per capita of about $4,000, mobilized all its social resources to suppress the virus and had only a single death. The world does not need more Canada. It needs more Bhutan.
And the provinces didn’t necessarily need more Ottawa. From time to time during the pandemic, people called for the federal government to invoke the Emergencies Act to force the provinces to do a better job. Given federal failures in its areas of jurisdiction, there is no reason to assume the feds are better able to handle difficult tasks than the provinces. Ottawa failed to warn Canadians about the impact of the virus, failed to maintain a stock of PPE, bungled the return of the snowbirds and couldn’t manage call centres for Canadians who needed to arrange hotel quarantines. A lot of feds apparently just stopped working during this crisis: the Canadian Press reported that a third of civil servants got paid time off work, on grounds that they couldn’t work remotely, at a cost of more than $800 million.
An important lesson of the pandemic is the success of the East Asian democracies. Taiwan, South Korea and Japan all did much better than we did. I suspect part of the reason is they do not accept repeated failures by their public service.
An email released to the Commons health committee illustrates the approach our political class takes to these things. After the Globe and Mail revealed that PHAC had foolishly taken vital resources away from our pandemic early warning system, a staffer in the PMO emailed a colleague to point out that the political people weren’t responsible: “those would be internal, bureaucratic decisions, not political ones.” The government didn’t mean to dismantle our pandemic alarm system, in other words. It happened, as many things do, secretly, apparently without the knowledge of our elected representatives, who might have found out about it if they were interested. But it was not the government’s fault. Federal bureaucratic institutions are reflexively secretive, because openness leads to accountability. MPs of all stripes put up with this, often because it doesn’t serve their partisan ends either to delve into the details.
The provincial record was no better. It may be bad luck that the pandemic, which hit cities hardest, happened when all the provinces from Quebec to Alberta were governed by parties dominated by rural caucuses. Caught between public health advice and a desire to please voters bridling at restrictions, they opted for “balance,” which meant ineffective measures, which led to more contagion, more restrictions, more deaths.
There is reason to fear that worse pandemics lie ahead. Mike Ryan, the Irish doctor in charge of WHO’s emergency response to COVID—who eloquently warned leaders to be proactive back in March 2020—warned in February 2021 that, because of climate change, we are creating the conditions in which epidemics flourish. “We’re writing cheques we cannot cash as a civilization for the future,” he said. “Someday when we are not here, our children will wake up in a world where there is a pandemic that has a much higher case fatality rate, and that could bring our civilization to its very knees.”
It would be nice to think we would learn from this and be better prepared for that next, inevitable threat. After Ottawa mismanaged the Spanish flu, Vincent Massey called for the establishment of a federal health department, and the government responded. We can likely count on governments responding to this disaster, too, with new measures that will improve our resilience, but none of the fixes will be eternal. Our governments are run by politicians, whose primary goal—however much they talk about making decisions for the right reasons—is winning votes, for the excellent reason that they can’t do anything if people don’t vote for them.
Responding to catastrophes is better politics than preventing them. A 2009 paper by American political scientists Andrew J. Healy and Neil Malhotra analyzed American electoral history in regards to natural disasters. The professors learned that voters reward incumbent politicians for spending money on disaster relief but not for disaster preparedness, because voters are myopic and do not have the attention span to insist on wise measures, like public health.
After COVID, as in the years after SARS, that will no doubt change, for a while, and we will invest in public health. And then our attention will wander, people will forget, we will get on with our lives. With any luck, there will be a hedonistic period of pleasure-seeking when the virus is gone—as there was after the Spanish flu—and we will try to put this long, tedious year out of mind.
I hope when we remember it we will recall not just the isolation and suffering, but also the people who were doing what they could to help one another. There were a lot of those people, and the good they did made a huge difference: health-care workers who slept in the garage rather than risk infecting their families; frontline workers, volunteers and Canadian Armed Forces personnel who bravely risked contagion and PTSD in hellish LTCs; people who made thousands of masks for frontline workers; the silent majority who dutifully complied with public health guidelines and stayed isolated for months.

Health-care workers outside Women’s College Hospital in Toronto (Jay Watts)
In April 2020, when I called David Fisman to talk to him about the then-lively debate about masks, he mentioned something heartening, about the support he and other health workers were getting. When he was working long hours on models to show the public how the pandemic would move, friends would drop by with soup or samosas. “We have a friend who works in the catering industry. She’s been hitting us up repeatedly now to say, ‘Well, who do you know who works in intensive care units? Cause we want to deliver them some hot meals.’ ”
Fisman and I got to talking about how this pandemic compared to the Spanish flu, what life must have been like at a time when people were more accustomed to mass death than we are now, and about the lessons plagues teach us. Fisman opened his copy of Camus’s The Plague, the book I’d listened to on my drive home from Florida. A beautiful and difficult novel, it explores the suffering of a town beset by disease, and the love and solidarity that arises in the face of that suffering. There was a passage Fisman wanted to read aloud. He flipped to the last page and found it: “Dr. Rieux resolved to compile this chronicle, so that he should not be one of those who hold their peace but should bear witness in favour of those plague-stricken people; so that some memorial of the injustice and outrage done them might endure; and to state quite simply what we learn in a time of pestilence: that there are more things to admire in men than to despise.”
—with files from Marie-Danielle Smith, Nick Taylor-Vaisey and Jason Markusoff
Editor’s note:
We hope this article added to your understanding of how the pandemic unfolded in this country.
But quality journalism is not free. It’s built on the hard work and dedication of professional reporters, editors and production staff. We know this crisis may be taking a financial toll on you and your family, so we do not make this ask lightly. If you are able to afford it, a Maclean’s print subscription costs $6 for the first six months — and in supporting us, you will help fund quality Canadian journalism in this historic moment.
Our magazine has endured for 116 years by investing in important stories and great writing. If you can, please make a contribution to our continued future and subscribe to our print edition here.
Thank you.
Alison Uncles
Editor-in-Chief, Maclean’s

https://www.facebook.com/druthers.net/videos/422630819548578
Druthers News & Information was live.
- 2:13:28Great to see so many people on the side of law and science pushing back against the cranks on here. Keep it up. The people are behind you.120:00Dominic Cardy from the conversations I see you are having, you are causing so much division in our province.. . Your policies remind me of what I have been reading about Nazi Germany and the hated they caused.. towards the Jewish people.. vaxxed or not vaxxed.. your hatred is appalling towards those who disagree with you. Very poor example of humanity.13You're a hateful divisive man and you should be ashamed of yourself. How you advocate for suffering on people of this province is truly appalling. I don't know how you sleep at night.650:00Dominic Cardy Yo Cardy when may I expect the Fat Fred City Finest to return my Harley and some more butter tarts from you and Higgy???
Conversation
Dominic Cardy
Dominic Cardy’s Tweets
Who to follow
 Chef/Leader:
Chef/Leader: 
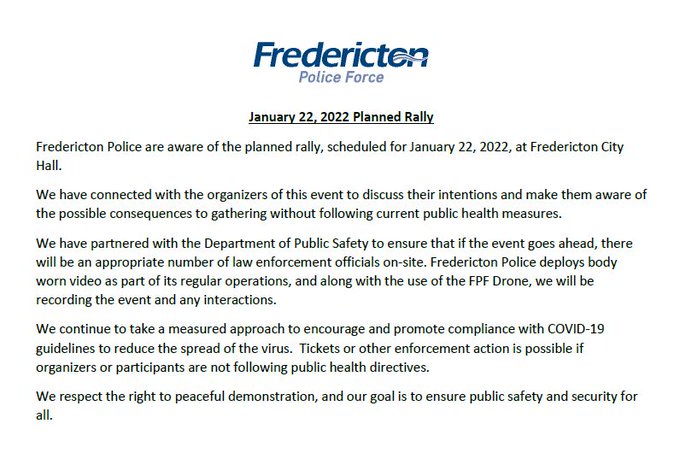





















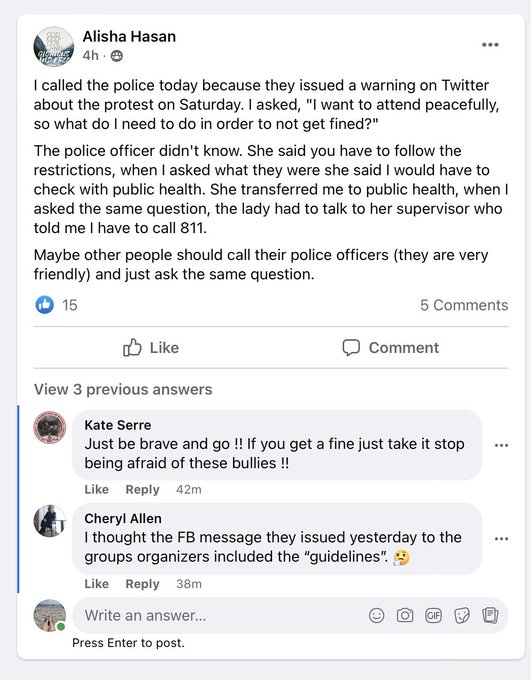








No comments:
Post a Comment